Busra Kaynar 1, Resmiye Ozdilek 2, Unal Turkay 3
1 Department of Midwifery, Kocaeli Provincial Directorate of Health Darica Farabi Training And Research Hospital, Gynecology and Obstetrics Midwifery, Kocaeli, Turkey.
2 Department of Midwifery, Faculty of Health Science, Kocaeli University, Kocaeli, Turkey.
3 Department of Gynecology and Obstetrics, Kocaeli Health and Technology University, Kocaeli, Turkey
Received: 7 May 2024
Revised: 10 May 2024
Accepted: 10 May 2024
Published: 10 May 2024
Corresponding author:
Resmiye Ozdilek.
Department of Midwifery, Faculty of Health Science, Kocaeli University, Kocaeli, Turkey. resmiyeozdilek@gmail.com
ABSTRACT
| Areolar secretions from breastfeeding women are particularly notable for newborn babies. This study evaluated the effect of sensing the mother’s areolar odor on newborn sucking success previous to being in contact with the mother. This study was a randomized controlled trial conducted with healthy newborns born by elective cesarean section (n:100). Those in the experimental group contacted breast pad having breast areolar odor taken from the mothers after cesarean section and before contact with their mothers. Routine interventions were administered to the control group: no pads were exposed to the mother’s scent. Physiological responses of the newborns in the experimental group who sensed the areolar odor had heart rates and intensity of crying significantly different from those in the control group. During the intervention, head orientation, oral movement/licking, and facial expression of newborns in the experimental group were significantly higher compared to those in the control group. The LATCH scale score was 8.78±0.737 in the experimental group, 6.88±0.961 in the control group; the difference was statistically significant. Duration of sucking in the first meeting with the mother was 22.42±5.06 minutes in the experimental group and 13.00±3.91 minutes in the control group. The difference in the duration of sucking between the groups was significant. Exposure of the newborn to areolar odor may increase breastfeeding success between caesarean section and first contact with the mother and prolong the duration of first breastfeeding. |
Keywords:
Areola, newborn, breastfeeding success, cesarean section, odor
Cite as:
Kaynar B, Ozdilek R, Turkay U. The Effect of Scenting Areolar Odor to the Cesarean Newborn on Sucking Success Before Meeting with the Mother: A Randomized Controlled Study. Acta Med Eur. 2024;6(3):65-73.
INTRODUCTION
Odor is the most developed sense that ensures emotional ties between mother and baby; it constitutes behavioral responses of newborns (1,2). The sense of smell is formed at 26–28 gestational weeks of fetal life. Like the other senses, smell also creates emotional and motor responses. The newborn might have orocephalic responses to odors such as coughing, sneezing and grimace (3). The fetus, being immersed with amniotic fluid in the early fetal period, continues to use this experience as of birth. The newborn has both physiological and behavioral responses to exposed odors. Studies conducted using odors indicate that newborns prefer a scented environment to an unscented and/or unknown environment. Newborns tend to be in environments with both familiar and confident odors (3,4). Newborns’ odor awareness is so powerful that they can detect their mother’s odor among many other odors. Studies have proved that infants respond to pleasant and familiar odors (5–9). Odors facilitate adaptation of the newborn and constitute part of the sense of attachment (10). Nipple odors give off hints to the newborn that allow them to follow the odor and find the breast (11,12). Studies indicate that areolar odor scent sensed by the newborn led them to cry less and facilitated their sucking/breastfeeding (2,7,8). Volatile compounds are excreted from the Montgomery tubercles located in the breast areola;they affect behavior of the newborn in several ways (8,13,14). Various odor substrates are locally elicited by colostrum, milk, and secretions of the areolar glands. Montgomery tubercles spread in the areola consist of sebaceous and lactiferous units, structures that expand during pregnancy and breastfeeding that elicit visible secretions (15). Studies also indicate that areolar odor positively affects orocephalic newborns’ responses (7,16–18). In the study by Varendi (2007), pads with breast odor were placed at a distance of 17 cm from the infants in the experimental group; pads without odor were used for infants in the control group. The infants tended to react toward pads with odor at a significantly higher rate than pads with no odor (19). This behavioral and autonomic response in newborns may stem from the fat and lacteal content of the Montgomery secretions (20).
Practices such as skin contact after birth provide odor activation in the newborn, whereas mother and baby are isolated; thus, mother’s odor and stimulation is delayed during cesarean section (21). It is very important to initiate breastfeeding in the active postpartum period (0–30 minutes) of the newborn. However, initiation of breastfeeding in cesarean section is delayed in current medical practice (22). Increasing the bonds between the mother and infant should be targeted postpartum (23). Prolongation of meeting with the mother post-cesarean section or mother’s fatigue and feeding the newborn other than breast milk because the mother needs rest due to her pain; this negatively affects breastfeeding activity and the initial bonds between the mother and infant (21). Being with the mother and scenting her odor allows the newborn to feel safe and relieve stress, however, in Turkey, there is no post-cesarean section routine where mother and baby meet or have skin contact. This is a very difficult process for the newborn’s first hours: these stress factors (light, sound, intervention, etc.) that the newborns confront during the adaptation period not only affects their adaptation to life but also negatively affect the bonds between the mother and infant (24). In this period, stress should be kept minimal and the newborn needs to be supported to adapt to life, so postpartum practices during the newborn’s adaptation process are important. In particular, studies have indicated that the breast milk odor has a soothing effect on the newborn, significantly increases orocephalic responses, and contributes positively during adaptation to life (3,9,19,25). In addition, breast milk odor is known to decrease respiratory distress and increase oxygenation (Marlier et al., 2005; Nishitani et al., 2009; Uraş & Akşit, 2017). Odor, particularly mother’s odor, is known to boost suction activity of the newborn, to decrease spontaneous crying, and to relieve pain (26).
Studies on odors familiar to the newborn areolar odor, amniotic fluid odor, and breast milk odor attracting them to the breast postpartum have shown that odor relieves the newborn, increases their orientation to life postpartum, and prepares them to suck (12,14,27). The present study aimed to determine suction success of the newborn by sensing the mother’s areolar odor when the meeting with the mother of the newborn was delayed due to medical necessities arising from cesarean section.
METHODS
Study hypotheses
H0: The “Areolar odor’ affects the newborn’s sucking success
H1: The “Areolar odor’ has no effect on newborn’s sucking success.
Study type
An experimental study with control group design was conducted between October 2019 and February 2020 in Kocaeli.
Location and characteristics of the study
This randomized controlled study comprised newborns of pregnant women admitted to the gynecology and obstetrics unit of the training and research hospital.
Population sample
The alpha was 0.05, the predicted difference in regard to the first breastfeeding time between the experimental and control groups was 60 minutes, the standard deviation was 3, and the power of the study was taken to be 80% through the power analysis done to calculate the sample size. In this analysis, the sample was determined to be 45 newborns and mothers for the experimental and control groups. Considering the possibility of dropout, a total of 50 newborn and mothers were included in the groups, and the study was completed with a total of 100 mothers and newborn, equally distributed in the groups (50 in the experimental and 50 in the control groups).
Personal Information Form
This form comprises a total of 14 questions involving sociodemographic and obstetric attributes.
Newborn Evaluation Form
This form comprises a table that includes gender, height, weight, head circumference, APGAR score information, time passed until suction, sucking time, vital findings, and orocephalic response measures.
The LATCH Breastfeeding Assessment Tool
The LATCH is a breastfeeding diagnostic and measurement tool developed by Jensen et al. in 1993 (28). The LATCH scale includes five evaluations: holding breast, swallowing action of the infant, nipple, mother’s comfort, and holding position of the infant. Each criterion is scored 0, 1, and 2 in the measurement tool: the lowest obtainable score is 0 and the highest is 10. A higher score is directly proportional to the sucking success, and a score of at least 7 shows breastfeeding was successful. The Cronbach’s alpha value forthis study was 0.86.
Tools and Materials
UNI-T UT 353 Mini Digital Sound Level Meter Decibel meter device®: This was used to measure the sound level of the newborn while crying.
Baby Neo Bamboo Washable Breast Pad Neo Comfort®:
This is a washable breast pad made of bamboo with no odor or color; it is round in shape and odor-retaining, with a watertight layer.
Collection of Data (Patient selection and randomization)
The inclusion criteria for the study were born at term, weight 2500–4000 g, an 8–10 APGAR score for the newborn, no obstetric risk, and voluntary participation of the pregnant woman. The exclusion criteria were low birth weight, APGAR score below 8, and being unwilling to participate.
Potential factors (gender, parity, type of anesthesia) that could affect the newborn’s suction were considered; randomization to the groups was done using a stratified sampling and blocking method (29). The researcher randomized the newborn to the groups by lottery based on being male/female, primipara/multipara, and general anesthesia/spinal anesthesia.
Intervention
The pregnant women who were at term in their pregnancy and hospitalized for elective cesarean were each given two Bamboo Breast Pad® in eight hours prior to the operation. They were instructed to place the bamboo pads to cover the breast areola, not to use any substance with odor (perfume, shower gel, soap, lotion, etc.) that might blend with body odor before and after placement. They were informed that the pads would be taken off the breast by the researcher prior to the cesarean section.
The researcher moved the breast pads prior to the operation and placed them in disposable zip lock transparent bags. Procedures for the postpartum first evaluations of the newborn and routine practices regarding the “Primary Care for the Newborn” of the Turkish Ministry of Health were followed (Figure 1).
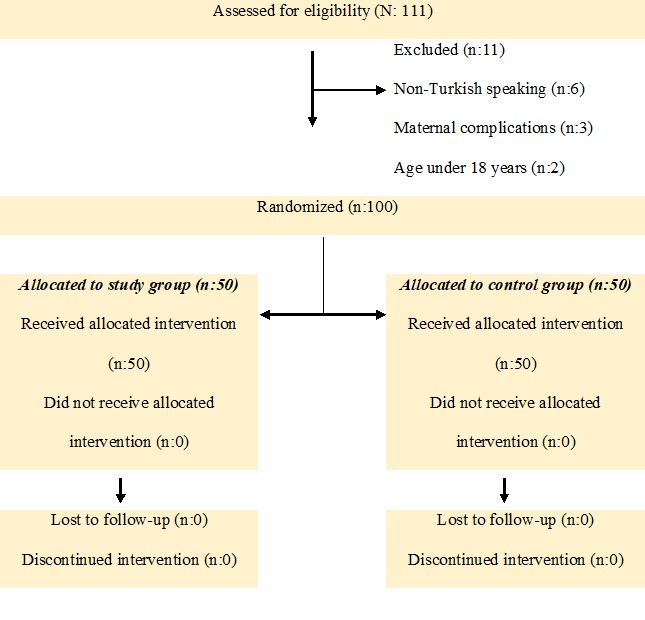
Figure 1. Consolidated Standards of Reporting Trials flow diagram of participants.
A transparent plexiglass mechanism previously warmed by a radiant heater was placed on the newborn’s head at 17 cm to attach the breast pads (Figure 2). Based on the study of Varendi that used mothers’ breast odor,the odor mechanisms were placed at 17 cm, which had been determined to be the distance at which a newborn could detect an odor and respond to it. Similarly, our study placed the pads at that distance in the mechanism because it used mother’s odor (19). Areolar odor pads taken from mothers were placed on the newborn in the experimental group, whereas unscented and unused pads were placed for the control group.
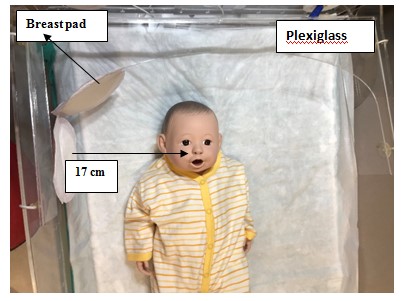
Figure 2. The mechanism used in the study showing its position relative to the newborn.
With the newborn in the odor mechanism, the intensity of crying, vital findings, and orocephalic responses were recorded. The duration that passed between the odor response test and the meeting of mother and newborn was recorded. The newborn was given to the mother for breastfeeding in that first meeting. The LATCH scale was used to evaluate the success of breastfeeding, and the total duration was of the first breastfeeding was recorded.
The data obtained from the study were entered in the computer and analyzed using SPSS 21.0 software that is used for statistical analyses in Kocaeli University. Whether the data fit normal distribution and the variances fit homogeneous distribution was evaluated by the researcher and a statistician. The t-test was used to compared continuous variables and the chi-square test was used to compare categorical variables of the experimental and control groups. The study used the Student’s t-test, Mann-Whitney U test, and Spearman’s (rho) correlation test to compare the dependent variable of the study, the LATCH scale score, with the independent variables in both groups. The Cronbach’s alpha value of LATCH was calculated with reliability analysis.
Ethical principles
- Ethical approval of the study was obtained from Saglik Bilimleri University Ethics Committee (28.11.2019/2019-129)
- Written permission was obtained from the Kocaeli Darıca Farabi Training and Research Hospital Chief Physician and Delivery Room Supervisor.
- Relevant training sessions were provided for the pregnant women who met the research criteria, provided their consent forms, and gave permission. Participation in the study was on voluntary basis through the information given and there was no forcing.
RESULTS
Study population
The mothers’ mean age was 27.9±5.81 in the experimental group and 28.2±6.75 in the control group. Of the mothers, 74% (n=37) in the control group and 78% (n=39) in the experimental group were multipara. The type of anesthesia performed in cesarean section was spinal anesthesia in 52% (n=26) and general anesthesia in 48% (n=24) in the experimental group; 50% (n=25) spinal anesthesia and 50% (n=25) general anesthesia in the control group. There was no significant difference between the experimental and control groups regarding gender and APGAR score of the newborn; the distribution was homogeneous (p>0.05) (Table 1).
Table 1. Findings from sociodemographic and obstetric attributes of mothers and newborns.
| Experimental Group (n=50) | Control Group (n=50) | Total (n=100) | Significance | |||||
| Mean Age | 27.9±5.81 min:18 max:43 | 28.80±6.75 min:18 max:42 | 28.35±6.28 min:18 max:43 | F=2.879 p=0.930 | ||||
| n | % | n | % | n | % | |||
| Age Groups | ||||||||
| 18 to 22 years of age 23 to 28 years of age 29 to 34 years of age 35 to 43 years of age Total | 11 20 10 9 50 | 11.0 20.0 10.0 9.0 100.0 | 12 13 11 14 50 | 12.0 13.0 11.0 14.0 100.0 | 23 33 21 23 100 | 23.0 33.0 21.0 23.0 100.0 | X2=2.663 p=0.447 | |
| Education Level | ||||||||
| Illiterate Primary school Secondary school High school University Total | 2 5 26 12 5 50 | 4.00 10.0 52.0 24.0 10.0 100 | 3 10 23 11 3 50 | 6.0 20.0 46.0 22.0 6.0 100 | 5 17 49 23 8 100 | 5.0 17.0 49.0 23.0 8.0 100 | X2=0.674 p=0.714 | |
| Income Level | ||||||||
| Less income than expense Equal income and expense More income than expense Total | 6 41 3 50 | 12.0 82.0 6.0 100 | 4 46 0 50 | 8.00 92.0 0 100 | 10 87 3 100 | 10.0 87.0 3.0 100.0 | X2=3.687 p=0.158 | |
| Parity | ||||||||
| Primipara Multipara Total | 13 37 50 | 26.0 74.0 100.0 | 11 39 50 | 22.0 78.0 100.0 | 24 76 100 | 24.0 76.0 100.0 | X2=0.219 p=0.640 | |
| Performed Anesthesia | ||||||||
| Spinal Anesthesia General Anesthesia Total | 25 25 50 | 50.0 50.0 100 | 26 24 50 | 52.0 48.0 100.0 | 51 49 100 | 51.0 49.0 100.0 | X2=0.40 p=0.841 | |
| Newborn genders | ||||||||
| Female Male Total | 26 24 50 | 52 48 100.0 | 25 25 50 | 50 50 100.0 | 51 49 100 | 51 49 100.0 | X2=0.040 p=0.841 | |
| APGAR Score of Newborns | ||||||||
| APGAR 1st minute | 8.86±0.35 min:8 max:9 | 8.86±0.35 min:8 max:9 | 8.86±0.35 min:8 max:9 | t=0.000 p=1.000 | ||||
| APGAR 5th minute | 9.96±1.96 min:9 max:10 | 9.98±1.98 min:9 max:10 | 9.97±1.97 min:9 max:10 | t=0.581 p=0.245 | ||||
| F:Levene’s Test for Equality of Variances; X2:Pearson’s Chi-Squared Test | ||||||||

Figure 3.Newborn’s response to areolar odor.
Response of the Newborn to Odor
There was no difference in the respiratory rate of the newborn in their response to odor at the 15th minute, whereas there was a significant difference in the intensity of crying, heart rate, head orientation, oral movement/licking and grimace (p<0.005) (Figure 3).
The duration of sucking of the experimental and control groups was compared and was found to be 22.42±5.06 (min: 10, max: 30) in the experimental group and 13.00±3.91 (min: 5, max: 20) in the control group. The difference in the duration of sucking between the groups was significant (p<0.05). This duration passed until the meeting of the mother and newborn was 45.90±4.70 (min: 40, max: 60) in the experimental group and 47.40±3.07 (min: 40, max: 55) in the control group (Table 2).
Table 2. Findings from the comparison of physiological and orthocephalic responses of the newborns in the experimental and control groups during the intervention.
| Experimental Group (n=50) | Control Group (n=50) | Significance | ||||
| Respiration 15th minute | 45.40±3.94 min:37 max:55 | 49.46±4.43 min:41 max:57 | t=1.046 p=0.309 | |||
| Heart Rate 15th minute | 136.50±9.86 min:118 max:154 | 147.80±5.33 min:135 max:158 | t=27.56 p=0.000 | |||
| Intensity of Crying 15th minute | 49.50±10.05 min:40 max:94 | 57.42±9.90 min:42 max:87 | t=14.65 p=0.000 | |||
| Experimental Group (n=50) | Control Group (n=50) | Significance | ||||
| Head Orientation 15th minute | n | % | n | % | X2/p | |
| Turning head to smell – Yes Turning head to smell – No Total | 48 2 50 | 96.0 4.0 100.0 | 4 46 50 | 8.0 92.0 100.0 | X2=77.564 p=0.000 | |
| Oral Movement/Licking 15th minute | ||||||
| Oral Movement/Licking – Yes Oral Movement/Licking – No Total | 47 3 50 | 94.00 6.0 100.0 | 3 47 50 | 6.00 94.0 100.0 | X2=77.440 p=0.000 | |
| Grimace 15th minute | ||||||
| Grimace – Yes Grimace – No Total | 35 15 50 | 70.0 30.0 100.0 | 0 50 50 | – 100.0 100.0 | X2=53.846 p=0.000 | |
| Duration of Sucking (minutes) | 22.42±5.06 min:10 max:30 | 13.00±3.91 min:5 max:20 | Z=-7.298 p=0.000 | |||
Table 3. Findings from the comparison of the LATCH scale scores in the experimental and control groups.
| Experimental Group (n=50) | Control Group (n=50) | Significance | |
| LATCH Total Score | 8.78±0.737 | 6.88±0.961 | t=6.231 p=0.000 |
| L-Breast Holding Sleeps or sucks involuntarily.Retries and latches the nipple.Holds the breast to latch the areola and sucks rhythmically. | 2.86±0.452 | 1.80±0.638 | t=12.056 p=0.001 |
| A-Seeing the Newborn Swallowing No swallowing action. A few actions of swallowing. Constant and strong inspiration is seen. | 2.94±0.239 | 2.08±0.528 | t=11.259 p=0.001 |
| T-Types of Nipples Inverted Flat It protrudes by stimulus | 3.00±0.00 | 3.00±0.00 | – |
| C-Comfort of Mother in Terms of Her Breast and Nipple There is engorgement, crack, bleeding and bruise. Tissue redness, minor bruises, decreased comfort. Soft breasts and comfort in mother. | 3.00±0.00 | 3.00±0.00 | – |
| H-Newborn Holding Position Completely needs help. Minimum help.No help. | 1.98±0.318 | 2.00±00 | t=7.901 p=0.006 |
t=Independent Sample t-test
Sucking success
The LATCH scale score measured during the meeting of the mother and newborn was significantly high (p=0.000). The value of L (breast holding evaluation) was p=0.001 in the control group, which was significant. The value of A (seeing the swallowing action of the infant) was p=0.001, which was significant. There was no significance in terms of T (type of nipples), C (comfort of mother in terms of her breast and nipples). The value of H (newborn holding position) was p=0.006 in both the experimental and control groups, which was significant (Table 3).
DISCUSSION
Our study found that the newborns in the experimental group who scented areolar odor had a lower heart rate (Table 3). The literature suggests that odor has a soothing effect on the newborn. The study of Tasci conducted on the soothing effect of breast milk odor on the newborn showed that heart rates of these infants were lower (25). Another study investigated the newborn response to odor scented during heel lance. Whereas in that study the intervention groups encountered scents of breast milk, lavender, and amniotic fluid, the control group infants were exposed to no scents. The researcher stated that heart rates of the newborn in the intervention group post-operation were lower than those of the control group (30). Similarly, a total of 84 newborns were included in the study on neonatal pain during heel lance. Tasci and Ayyildiz measured the heart rates of newborns who encountered scented breast milk and formula milk before, during, and after heel lance blood collection. The newborns who encountered scented breast milk had lower heart rates (25). Porter et al. determined that areolar odor and amniotic odor soothed newborns and affected their heart rates (31). Another study stated that the newborn experiencing breast milk scent calmed down, and physiologically, their heart rates and mobility decreased (2). In light of these findings from the literature that areolar odor, breast milk, amniotic fluid odor, and maternal odor decreased heart rates in the newborn, previous studies support the present study’s results.
Our study found that in the experimental group newborns’ intensity of crying after exposure to areolar odor was significantly lower than crying intensity of the control group. A study examined the pain response and stress levels of 48 newborns exposed to breast milk scent. Those researchers stated that the newborns exposed to breast milk scent had less intensity of crying and lower salivary cortisol levels (3). A study indicated that the newborns exposed to breast milk scent had lower duration of crying (25). Duration and intensity of crying of newborns exposed to various odors in invasive procedures were lower when exposed to familiar odors such as breast milk and maternal odors (32,33). The study of Sullivan and Toubas conducted on the soothing effect of maternal odor concluded that maternal odor reduces stress factors and reduces the duration of crying (2). Based on this information from the literature, the lower intensity of crying in newborns in response to areolar scent in our study can be attributed to the soothing effect of maternal odor.
The sense of smell is one of the most important senses creating a link between the mother and newborn. This important sense begins to develop in the intrauterine environment (14). Studies have shown that the sense of smell develops further after birth and is activated by clearing amniotic fluid and mucus from the nose (9,34). The newborns in our study had increased head orientation toward pads containing areolar odors.
The study of Porter and Winberg showed that head orientation of the newborn to breast odor was intentional (31). The study of Varendi and Porter conducted on the reach of the newborn to pads containing areolar odor consisted of 22 newborns who were laid on a level surface in prone position; pads were placed at a distance of 17 cm from them, the authors observing as the newborns reached toward these pads. The duration of reaching the pads with areolar odor was less compared to pads with no odor (19). In a study conducted on newborns at days 2 and 4, the newborns were exposed to their mother’s amniotic odor, the amniotic odor of another mother, and colostrum odor. The newborns had a head orientation toward their own mother’s amniotic odor, which is known to have similar content to that of breast odor they are familiar with (35). In a study conducted in Japan, the newborns were exposed to breast pads both with odor and with no odor. Their head orientation was toward pads with areolar odor, and they easily distinguished their mother’s breast pads soaked in their mother’s milk from other pads by a week after their birth (19). A study exposing the newborn to breast milk and vanilla showed that they had greater head orientation toward the breast milk (36). It’s been found that nipple odors give off hints to the newborn that allows it to orient itself toward the odor and find the breast (11,12). Could be said that breast odor alone, independent of any stimulation or support, is a very powerful source that attracts the newborn to the breast. As seen in the relevant literature, newborn have a high head orientation toward breast odor. Significant head orientations of newborn toward scented areolar odors in our study are similar to results in the literature.
Oral movements of the newborn in the experimental group were significant compared to those in the control group. Many studies in the literature have investigated responses of the newborn to odor. The newborns stimulated with areolar odor open their eyes, tend to the breast, and show behavioral and autonomic responses like licking and seeking. Researchers believe that this response is related to the fat and lacteal content of the Montgomery secretion (5,7,15). Benoist et al. reported that the licking and mouth-opening movements shown by the newborn that experienced the areolar scent were significantly higher than that in the control group (37) A study conducted to determine the effect of olfactory experiences in an amniotic environment on postpartum selective reactivity of the newborn has shown that the sense of smell begins in the amniotic environment. The preparatory mechanisms related to the feeding odor lead to an increase in behaviors such as tending to the breast, licking and seeking (38).
The behavioral responses of 3–4 day newborns were investigated by exposing them to their own mother’s milk, another mother’s milk, and formula milk. Newborns have significantly higher mouth movements and reactions to the breast milk odor of their own mothers (7).
A study examining the effect of maternal odor on pre-sucking responses reported that the newborn reacted to their mother’s odor, showing behaviors like increased mouth movements and tranquility (2). The results of the studies conducted support our study results.
There was a statistically significance in our findings regarding the comparison of the newborns’ facial expression of the experimental and control groups. In the study of Rattaz et al. conducted on soothing feature of familiar odors for the newborns, the infants were exposed to breast milk, vanilla, unfamiliar odors, and to materials with no odor. The researchers concluded that newborns responded to breast milk odor with facial expressions (39).
In a study on 48 newborns, the infants were exposed to their mother’s breast milk, breast milk of another woman, and formula milk to evaluate their motor activities in painful interventions, facial expressions, and crying. The newborns who smelled their own mother’s breast milk odor were more comfortable in painful interventions and showed less grimacing and disgust signs in their facial expressions (3).
Jessen’s study investigated the effects of maternal odor on emotional responses in the infant’s brain. The electroencephalographic (EEG) examination showed that emotional responses of the infants were calmer when they were exposed to maternal odor (40). A study using breast pads with maternal odor examined newborns’ responses to the odor. It reported an increase in tendency and in physical response to the pads with maternal odor. The results of the study showed that only maternal odor was found to be sufficient to attract and direct the newborn (19). Soussignan et al. investigated the autonomic responses of the newborns to maternal and milk odors and reported an increase in their facial expressions and autonomic responses to familiar odors (36). A study observing the newborns’ reactions to painful interventions found that those newborns who smelled breast milk were calmer and their facial expressions increased positively (3). Overall, studies show that newborns respond with positive facial expressions to maternal odor, breast milk odor, and familiar odors. Our study finding that facial expressions of the newborns in the experimental group who smelled pads with breast odor were significantly higher than the control group is similar to other studies in the literature.
Sucking success is affected by many factors. Many factors like cesarean section, increased duration of separation of the mother and infant after cesarean section, and the effect of anesthesia on the mother negatively affect breastfeeding (41). In our study, the time passed until contact with the mother was 45–47 minutes in the study group. In the first suckling after contact with the mother, the newborns in the experimental group sucked milk for 22.42±5.06 minutes on average and the control group sucked milk for 13.00±3.91 minutes on average. Despite the difference in the newborns’ duration of sucking, they should suck at least for 10 minutes at the first meeting (42). Our study found that duration of sucking was significantly high in the experimental group exposed to areolar odor. Many studies have reported that areolar odor positively affects physiological and orocephalic responses in newborns, increases movements such as licking, mouth opening, and preparing for sucking; thus it is effective tending to and finding the breast (2,8,12,19,40,43–45).
This finding means that the newborns who experienced areolar odor until meeting with the mother are stimulated and that the odor increases the duration of sucking.
In the first contact between mother and infant, the LATCH score was found to be significantly high in the experimental group. A score of 7 points or more on the LATCH scale is deemed good sucking success (28). Sucking success is good for the experimental group and borderline for the control group, based on their mean scores. In the studies investigating the sucking success from mothers who gave birth by cesarean section, the LATCH scores were significantly lower than those who gave vaginal birth (41,46).
In the evaluation of L (breast holding), A (observing the newborn swallowing) of the LATCH scale, the mean score of the experimental group was significantly higher, whereas H (newborn holding position) was significantly higher in the control group. The LATCH breastfeeding success includes evaluation of the newborn, mother, and breast. The two items regarding breast holding and seeing the newborn swallowing are evaluations of the infant. The LATCH total score of the newborns in the experimental group was significantly higher than for those in the control group. The literature shows that areolar odor has an effect on attracting the infant to the breast, finding the breast, and preparing to suck (15,37,47). Doucet et al. covered the breast areola with a transparent film and observed the newborns holding and sucking mother’s breast. They reported that the newborns tended to hold and suck the uncovered breast more (37). We believe that scenting pads with areolar odor to the newborns until contact with the mother prepares them to suck. The significant difference in the LATCH scale items regarding the newborns in the experimental group indicates that the effect of areolar odor increases sucking success. Based on the findings from this study, exposing newborns to areolar odor increases sucking success between the cesarean section and the initial contact with their mothers and increases the duration of sucking.
The research findings are limited to the newborns in the hospital where the research was conducted and cannot be generalized to all newborns. The data obtained is limited to the evaluations of the scales used.
CONCLUSIONS
Based on the evaluation of the data obtained from the study, some suggestions have been made.
- In case of a delay in contact between mother and newborn due to cesarean section, the newborn should be exposed to areolar odor for preparation to the contact and for sucking.
- The midwives and nurses should be informed that areolar odor calms down, prepares the newborn for sucking, and contributes positively to physiological and orocephalic responses.
- The midwives and nurses should collaborate with the physician in elective cesarean section to provide areolar odor from the mother.
- Pregnant women should be informed about areolar odor while considering elective cesarean section.
- Scientific information should be provided regarding newborn response to areolar odor in in-service training of midwives and nurses.
- Further studies can be done with different sample groups in which mothers and the newborns are separated due to cesarean section.
- The effect of areolar odor can also be investigated when medical reasons other than cesarean section require separation of the mother and baby.
REFERENCES
- Daly KJR. The Role of the ECMO Specialist Nurse (2017). Qatar Medical Journal. 2017;54 doi: 10.5339/qmj.2017.swacelso.54
- Sullivan R, Toubas P. Clinical Usefulness of Maternal Odor in Newborns: Soothing and Feeding Preparatory Responses. Biol Neonate. 1998;74(6):402–408.
- Nishitani S, Miyamura T, Tagawa M, et al. The calming effect of a maternal breast milk odor on the human newborn infant. Neurosci Res. 2009;63(1):66–71.
- Kawakami K, Takai-Kawakami K, Okazaki Y, Kurihara H, Shimizu Y, Yanaihara T. The effect of odors on human newborn infants under stress. Infant Behav Dev. 1997;20(4):531–535.
- Bartocci M, Winberg J, Ruggiero C, Bergqvist LL, Serra G, Lagercrantz H. Activation of olfactory cortex in newborn ınfants after odor stimulation: A functional near-infrared spectroscopy study. Pediatr Res. 2000;48(1):18–23.
- Schaal B, Marlier L, Soussignan R. Olfactory function in the human fetus: Evidence from selective neonatal responsiveness to the odor of amniotic fluid. Behav Neurosci. 1998;112(6):1438–1449.
- Marlier L, Gaugler C, Messer J. Olfactory stimulation prevents apnea in premature newborns. Pediatrics. 2005;115(1):83–8.
- Varendi H, Porter RH, Winberg J. Does the newborn baby find the nipple by smell? Lancet. 1994;344(8928):989–990.
- Schaal B. Olfaction in infants and children: Developmental and functional perspectives. Chem Senses. 1988;13(2):145–190.
- Ince T, Kondolot M, Yalçin SS, Yurdakök K. Breastfeeding consultation status of mothers. J Child Heal Dis. 2010;53(3):189–197.
- Schaal B, Marlier L, Soussignan R, Nouzilly F, Bourgogne U De, Picardet RA, et al. The Anterior Insular Cortex Represents Breaches of Taste. Chem Senses. 2000;25(22):729–737.
- Schaal B, Al Aïn S. Chemical signals “selected for” newborns in mammals. Anim Behav [Internet]. 2014;97:289–99. Available from: http://dx.doi.org/10.1016/j.anbehav.2014.08.022
- Bengtsson S, Berglund H, Gulyas B, Cohen E, Savic I. Brain activation during odor perception in males and females. Neuroreport. 2001;12(9):2027–2033.
- Loos HM, Reger D, Schaal B. The odour of human milk: Its chemical variability and detection by newborns. Physiol Behav [Internet]. 2019;199(October 2018):88–99. Available from: doi: 10.1016/j.physbeh.2018.11.008
- Doucet S, Soussignan R, Sagot P, Schaal B. The secretion of Areolar (Montgomery’s) glands from lactating women elicits selective, unconditional responses in neonates. PLoS One. 2009;4(10).
- Bingham PM, Abassi S, Sivieri E. A pilot study of milk odor effect on nonnutritive sucking by premature newborns. Arch Pediatr Adolesc Med. 2003;157(1):72–75.
- Fox K. The Smell Report An overview of facts and findings. Soc Issue Res Cent. 2006;33.
- Stuck BA, Stieber K, Frey S, Freiburg C, Hörmann K, Maurer JT, et al. Arousal responses to olfactory or trigeminal stimulation during sleep. Sleep. 2007;30(4):506–510.
- Varendi H, Porter RH. Breast odour as the only maternal stimulus elicits crawling towards the odour source. Acta Paediatr Int J Paediatr. 2001;90(4):372–375.
- Doucet S, Soussignan R, Sagot P, Schaal B. An overlooked aspect of the human breast: Areolar glands in relation with breastfeeding pattern, neonatal weight gain, and the dynamics of lactation. Early Hum Dev. 2012;88(2):119–128. doi: 10.1016/j.earlhumdev.2011.07.020
- Keten E. Skin to Skin Contact and Breastfeeding After Cesarean Section. Univ Heal Sci J Nurs. 2021;3(2):103–108.
- Gunay I. Sezaryen Sonrası Emzirme. Hemşirelikte Eğitim ve Araştırma Derg. 2011;8(1):28–30.
- Unver R. Differentiation of Sense of Smell and Assessment of Diversity in Evolutionary Perspectives. Uludağ Univ Fac Arts Sci J Soc Sci. 2018;19(35):743–756.
- Akin Ö, Erbil N. Breastfeeding and Mode of Delivery: A Systematic Review. Ordu Univ J Nurs Stud. 2020;3(3):302–318.
- Tasci B, Kuzlu Ayyildiz T. The Calming Effect of Maternal Breast Milk Odor on Term Infant: A Randomized Controlled Trial. Breastfeed Med. 2020;15(11):724–730.
- Logan D, Brunet L, Webb W, Cutforth T, Ngai J, Stowers L. Learned recognition of maternal signature odors mediates the first suckling episode in mice. Curr Biol. 2013;22(21):1998–2007.
- Varendi H, Porter RH, Winberg J. Natural odour preferences of newborn infants change over time. Acta Paediatr Int J Paediatr. 1997;86(9):985–990.
- Jensen D, Wallace S, Kelsay P. LATCH: A Breastfeeding charting system and documentation Tool. J Obstet Gynecol Neonatal Nurs. 1994;23(1):27–32.
- Ozdemir O. Randomization. İku Derg. 2009;23:32–41.
- Akcan E. The effect of amniotic fluid, breast milk and lavender scent on pain during heel pricking in newborns. Erciyes University Institute of Health Sciences Kayseri; 2014.
- Porter RH, Winberg J. Unique salience of maternal breast odors for newborn infants. Neurosci Biobehav Rev. 1999;23(3):439–449.
- Yilmaz F, Arikan D. The effects of various interventions to newborns on pain and duration of crying. J Clin Nurs. 2011;20(7–8):1008–1017.
- Yilmaz G, Gurakan B, Saatci U. Factors influencing the duration of crying of infants after heel lance. Journal of Child Health and Diseases. 2002:232–236.
- Sullivan RM, Taborsky-Barba S, Mendoza R, Itano A, Leon M, Cotman CW, et al. Olfactory classical conditioning in neonates. Pediatrics. 1991;87(4):511–518.
- Marlier L, Schaal B, Soussignan R. Neonatal responsiveness to the odor of amniotic and lacteal fluids: A test of perinatal chemosensory continuity. Child Dev. 1998;69(3):611–623.
- Soussignan R, Schaal B, Marlier L. Olfactory alliesthesia in human neonates: Prandial state and stimulus familiarity modulate facial and autonomic responses to milk odors. Dev Psychobiol. 1999;35(1):3–14.
- Doucet S, Soussignan R, Sagot P, Schaal B. The “smellscape” of mother’s breast: Effects of odor masking and selective unmasking on neonatal arousal, oral, and visual responses. Dev Psychobiol. 2007;49(2):129–138.
- Schaal B. How amniotic fluid shapes early odor-guided responses to colostrum and milk (and more). In: Flavor. Elsevier; 2016. p. 23–53.
- Rattaz C, Goubet N BA. The calming effect of a familiar odor on fullterm newborns. J Dev Behav Pediatr. 2005;26:86–92.
- Jessen S. Maternal odor reduces the neural response to fearful faces in human infants. Dev Cogn Neurosci [Internet]. 2020;45:100858. Available from: doi: 10.1016/j.dcn.2020.10085841.
- Çakır D, Alparslan Ö. Examining the Effects of Child Type Variable on Mother-Baby Interaction and Mother’s Perception of Her Baby. Contemp Med. 2018;8(2):139–147.
- Kültürsay N, Bilgen H, Türkyılmaz C. Guide to feeding a healthy term baby. Turkish Neonatology Association. 2014;18:24–28.
- Doucet S. Contribution à l’étude des glandes aréolaires chez la femme: description morphologique, et corrélats fonctionnels dans l’adaptation mère-nouveau-né. Université Paris-Nord Paris. 13; 2008.
- Doucet S, Soussignan R, Sagot P, Schaal B. The “smellscape” of mother’s breast: Effects of odor masking and selective unmasking on neonatal arousal, oral, and visual responses. Dev Psychobiol. 2007 Mar;49(2):129–138.
- Schaal B, Doucet S, Sagot P, Hertling E, Soussignan R. Human breast areolae as scent organs: Morphological data and possible involvement in maternal-neonatal coadaptation. Dev Psychobiol. 2006;48(2):100–110.
- Yaşar Kivik S, Kürtüncü M. The effect of early skin-to-skin contact on breastfeeding in primipara mothers who gave birth with epidural anesthesia. Aegean Faculty of Nursing Journal. 2019;35(2):37–47.
- Porter R, Winberg J. Unique salience of maternal breast odors for newborn infants. Neurosci Biobehav Rev. 1999;23(3):439–449
