Semra Dogan 1, Salih Mujdat Balkan 2, Ibrahim Tanzer Sancak 3
1 Department of General Surgery, Yuksek Ihtisas University, Faculty of Medicine, Live Hospital, Ankara, Türkiye.
2 Department of General Surgery, Near East University, Faculty of Medicine, North Cyprus Turkish Republic
3 Department of Radiology, TOBB Economy and Technology University Hospital, Ankara, Türkiye
Received: 17 April 2024
Revised: 22 April 2024
Accepted: 22 April 2024
Published: 22 April 2024
ABSTRACT
| Gallbladder (GB) duplication is a rare congenital anomaly with various anatomical presentation. Preoperative diagnosis of this condition is not common as it is available in only 50% of cases. When problems arise, such as cholecystitis, this anomalies are exposed during an operation. We report the case of a double GB which was diagnosed during the operative procedure in fifty-seven years old woman with sign and symptom of acute cholecystitis. The liver function tests were elevated and ultrasonography showed the lithiasic cholecystitis in GB which rolled around itself. Magnetic Resonance cholangio pancreatography (MRCP) confirmed the cholecystitis on GB and revealed normal common bile duct(CBD). A decision was made to procedure with a laparoscopic cholecystectomy. Inoperative double gallbladder and double cystic duct was observed. Cholangiography was made to identify the biliary tree. A challenging laparoscopic cholecystectomy was performed successfully and pathology confirmed double H-type GB and cholecystitis on both of them. The patient was discharged home uneventfully. GB duplication has an incidence of approximately 1:4000. It can be classified as a type-I anomaly(partially split primordial gallbladder), a type II anomaly(two separate gallbladders, each with their own cystic duct) or a type III anomaly(triple gallbladders draining by 1-3 separate cystic duct). Such anatomical variations of the GB are associated with an increased risk of operative difficulty and complications including conversion to open cholecystectomy and common bile duct injury. Preoperative diagnosis of duplicate GB is difficult. This condition could not be detected preoperatively by imaging methods. During surgery, if surgeon suspects the presence of more then one cystic duct, intraoperative cholangiography is highly recommended to identify the biliary anatomy. |
Keywords:
Laparoscopic cholecystectomy, double gallbladder, double cholecystitis, gallstone
Cite as:
INTRODUCTION
Variations in biliary anatomy are frequently attained. Of these, gallbladder duplication is a very rare anomaly with an estimated incidence of approximately 1 in 4000 population (1). Preoperative imaging is often helpful for diagnosis of double gallbladder but it can miss up to 50% of cases (2). Congenital malformations are the most important predisposing factor for iatrogenic bile duct injuries during the laparoscopic cholecystectomy. If the intraoperative anatomy is not clear an intraoperative colangiogram should be performed (1,2). Here, we report a challenging laparoscopic cholecysistectomy for a double GB,which was an inta-operative diagnosed as the patient’s preoperative workup did not reveal any evidence of duplication of the gallbladder.
CASE REPORT
A fifty-seven year old woman patient referred to our outpatient clinic presented with a 3 days history of right upper quadrant pin and fever. The pain had been there for 1 month intermittently. She has no history of jaundice. Physical examination demonstrated tenderness to palpation in the right upper and lower quadrants; no organomegaly, palpable mass or jaundice were detected. Liver function tests identified marginally elevated AST (175u/L), ALT (215 u/L), GGT (928 u/L), direct bilirubin (3.48mg/dl)White blood cell (11590 u/L).
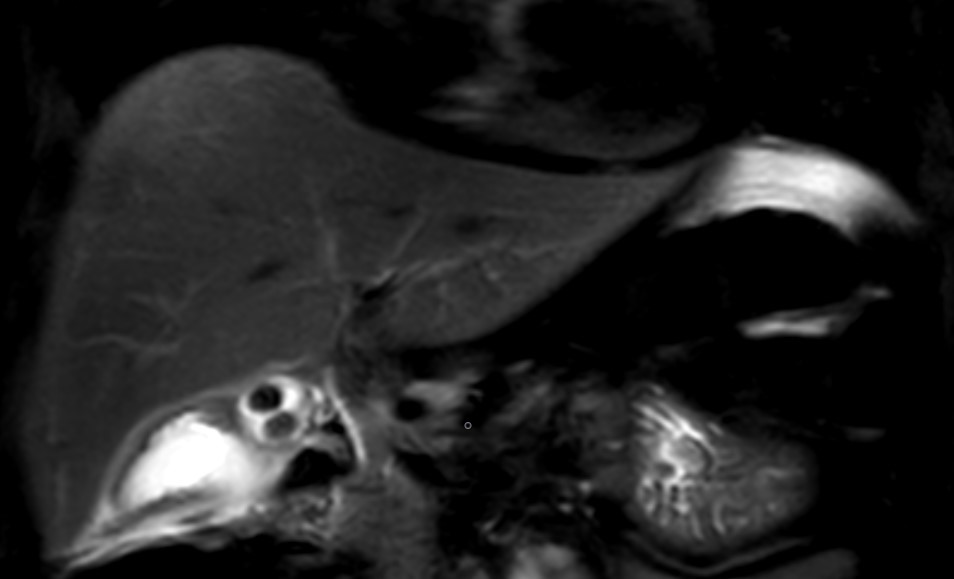
Figure 1. Two gallbladers and the stones in them, which can be seen in the T2 magnetic resonance image
Abdominal ultrasound (US) showed a thickened wall of gallbladder and the lithiasic cholecystitis in GB which rolled around itself. She was further investigated with Magnetic resonance cholangio pancreatography (MRCP), which confirmed the cholecystitis on GB which rolled around itself and revealed normal CBD (Figure 1). A decision was made to procedure with a laparoscopic cholecystectomy. Intaoperatively two gallbladders enveloped in a single peritoneal membrane and two cystic duct was observed (Figure 2). It was an operative suprize because her MRCP did not reveal any evidence of duplication of the gallbladder. Intaroperative cholangiography was decided to identify the biliary tree. This cholangiogram confirmed the presence of two cystic ducts opening in the CBD (Figure 3). After ligature of two separate cystic duct a challenging laparoscopic cholecystectomy was performed successfully.
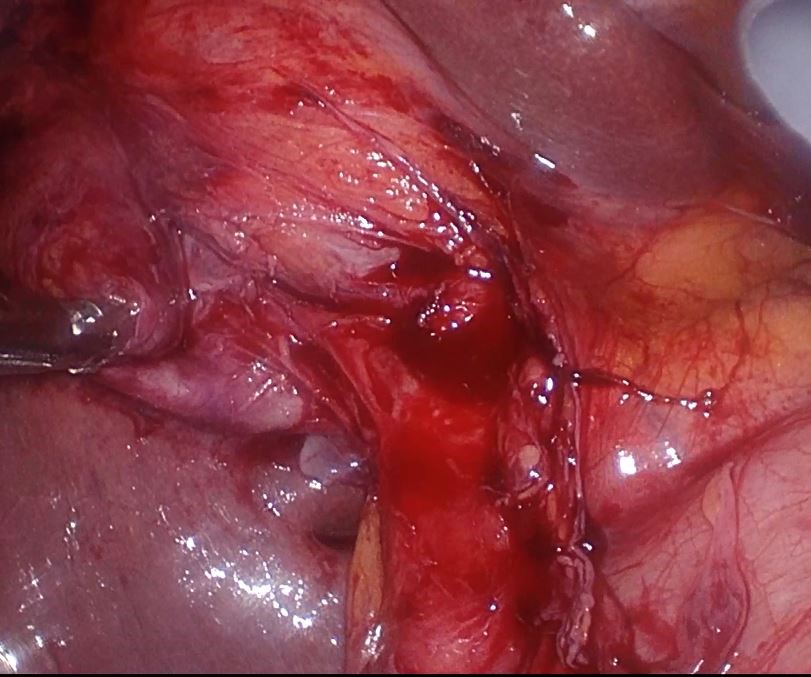
Figure 2 . Intraoperative image showind two gallbladers
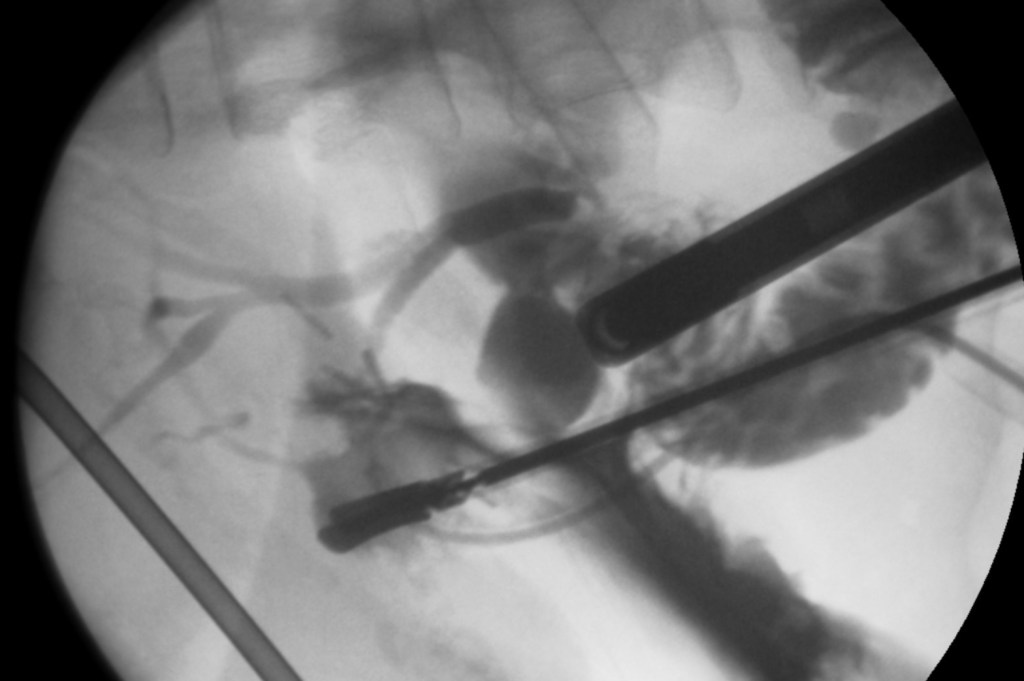
Figure 3. Intraoperative cholangiogram during cholecystectomy. Contrast demonstrates a normal common bile duct and intra hepatic ducts.
The patient had an uneventful recovery and was discharged home on postoperative day three. Inspection of the pathology specimen revealed a double H-type GB and chronic lithiatic cholecystitis on both of them (Figure 4). The patient was discharged home uneventfully.
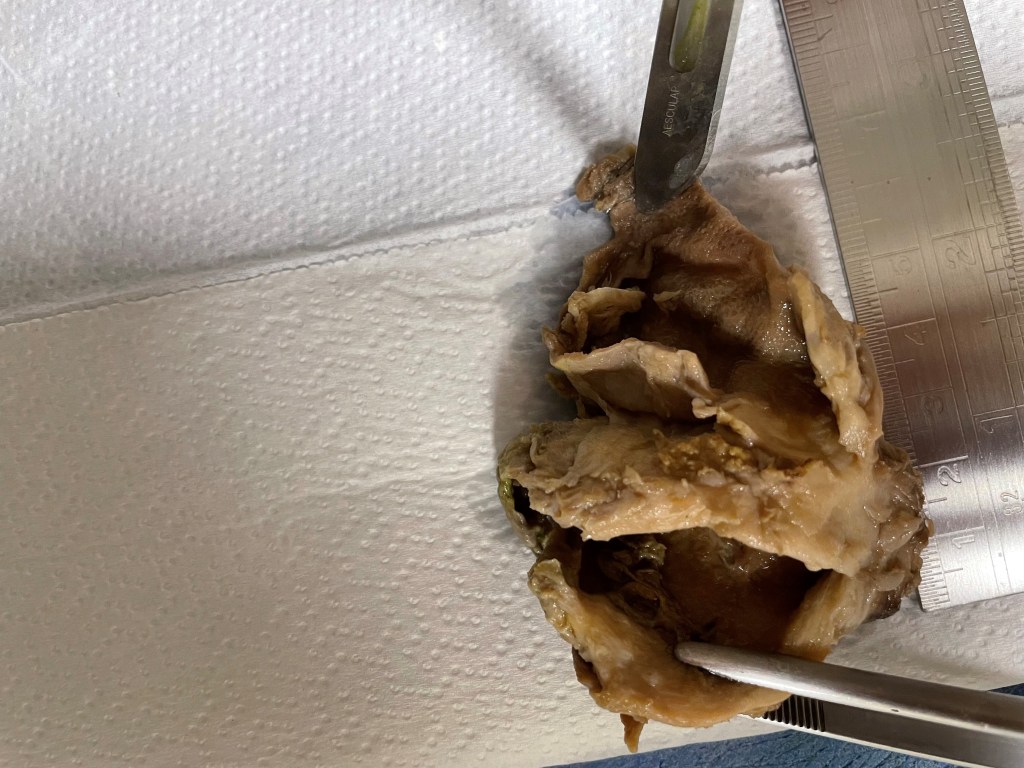
Figure 4. The operative piece of cholecystectomy showing two independent gallblader in a common peritoneal coat and each with seperate infindibulum.
DISCUSSION
Duplication of gallbladder was fist mentioned in 1974 when discovered upon autopsy by Blasius (5), the first mention of this anomaly in living patient was in 1911 by Sherren (6). In 1926 Boyden reported 20 cases of double gallbladder (1,2,5,6) and he described a system to classify gallbladder duplication including vesica fellea divisa (bilobed gallbladder with common neck and one cystic duct) and vesica fellea duplex (double gallbladder with two cystic ducts). Vesica fellea duplex is sub classified into H shaped type (two cystic ducts enter separately into the CBD), and Y shaped type (two cystic ducts unit before entering the CBD).
The most widely accepted is the Harlaftis classification published in 1977 (7). This classification separates two main groups (type 1and type 2) based on morphology and embriogenesis with respective incidence of 45.1% and 54.9%. In the type 1, shape of gallbladders can be septa ted or bi lobed (there is a single a septum that divides the two gallbladder), V-shaped (two separate gallbladders at the fundus but join at the neck) and Y shaped(two separate gallbladder each with a cystic duct combine to form one cystic duct before entering the CBD). In the type 2 called accessory GB there are more than one cystic duct joining the gallbladder with biliary tree. This type is further divided into ductular dublication or H type (two gallbladders each with a cystic duct entering separately into the CBD), and trabecular duplication (two separate gallbladder, the superior cystic duct enters the right hepatic duct). Kawanishi et.al concluded that the H-type was the most common (8). In our case represent Boyden vesica fella duplex H shaped, and Harlaftis type 2 ductular duplication.
There are no specific symptoms or signs associated with double gallbladder. Incidence of developing a biliary disease is no different in patient with double gallbladder than the one with a single gallbladder (9). Pillay, however, reported that the congenital malformation of the GB could cause a higher incidence of cholelithiasis due to inadequate drainage of bile (10).
Abdominal Ultrasound (US) can be helpful for preoperative diagnosis but the preoperative diagnostic accuracy of US can be as low as 50 % (11). The other diagnostic imaging method is computer tomography(CT) with the potential provide a good view of different intraluminal masses, although the literature shows it is not reliable in detecting biliary anomalies (12). MRCP have a higher sensitivity and specificity for showing the anatomy and variations of the biliary system (13). In our case MRCP revealed features of acute calculus cholecystitis in GB which rolled around itself at before the operation . But after the operation the radiologists did second look and they confirmed the double GB. Endoscopic retrograde cholangiopancreatography(ERCP) more precisely reveals the biliary anatomy but it is invasive procedure and it may not be indicated in every case of cholelithiasis or cholecystitis (12).
There is no role of prophylactic cholecystectomy in accidentally diagnosed cases. Surgical treatment should be perform only in symptomatic double GBs. Both GBs may be affected or one may be spared, however both lobes should be removed during surgery even if disease is present only in one to prevent subsequent disease in the remnant gallbladder at a later date (11-13).
Double GB could not be detected preoperative by imaging methots. During surgery, if surgeon encounter the unexpected biliary anomaly, intraoperative cholangiography is highly recommended to identify the biliary anatomy and complete a safe cholecystectomy.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Data availability statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
REFERENCES
- Bottari A, Fortuna L, Staderini F, Cianchi F, Coratti F. Duplication of the gallbladder in a patient with right colon cancer. A case report and review of the literature review. Ann Ital Chir. 2023;12:S2239253X23038689.
- Kim RD, Zendejas I, Velopulos C, Fujita S, Magliocca JF, Kayler LK, Liu C, Hemming AW. Duplicate gallbladder arising from the left hepatic duct: report of a case. Surg. Today 2009;39:536-539
- Gocmen R, Yesilkaya Y. Imaging findings of gallbladder duplication due to two cases: case report and review of literature. Med Ultrason. 2012;14(4):358–360.
- Y. Menu, M.P. Vuillerme, Non-traumatic abdominal emergencies: imaging and intervention in acute biliary conditions. Eur. Radiol. 2002;12:2397–2406.
- Baltaga L, Chrysikos D, Delis S, et al. Duplicated gallbladder: an incidental anatomical variation in a patient with symptomatic cholelithiasis. Folia Med (Plovdiv). 2023;65(5):834-838. doi:10.3897/folmed.65.e91397
- Zhou DK, Huang Y, Kong Y, Ye Z, Ying LX, Wang WL. Complete laparoscopic cholecystectomy for a duplicated gallbladder: A case report. Medicine (Baltimore). 2020;99(1):e18363. doi:10.1097/MD.0000000000018363
- Pera SJ, Huh N, Orcutt ST. Duplicate gallbladder: A case report of a patient with cholecystitis after cholecystectomy. Int J Surg Case Rep. 2019;65:156-160. doi:10.1016/j.ijscr.2019.10.075
- Kawanishi M, Kuwada Y, Mitsuoka Y, Sasau S, Mouri T, et al. A case of double gallbladder with adenocarcinoma arising from the left hepatic duct: a case report and review of the literature. Gastroenterol Res Pract. 2010;2010:721946.
- Desolneux G, Mucci S, Lebigot J, Arnaud JP, Hamy A. Duplication of the gallbladder. A case report. Gastroenterol Res Pract. 2009;2009:483473. doi:10.1155/2009/483473
- Pillay Y. Gallbladder duplication. International Journal of Surgery Case Reports, 2015;11:18-20.
- Hishinuma M, Isogai Y, Matsuura Y, et al. Double gallbladder. J Gastroenterol Hepatol. 2004;19(2):233–235.
- Cozacov Y, Subhas G, Jacobs M, Parikh J. Total laparoscopic removal of accessory gallbladder: A case report and review of literature. World J Gastrointest Surg. 2015;7(12):398–402.
- Adusumilli S, Siegelman ES. MR imaging of the gallbladder. Magn Reson Imaging Clin N Am. 2002;10(1):165-184. doi:10.1016/s1064-9689(03)00055-2
