Süleyman Akpınar 1, Özer İşisağ 2
1 Department of Material Science and Engineering, Afyon Kocatepe University, Faculty of Engineering, Afyonkarahisar, Türkiye
2 Department of Prosthodontics, Afyonkarahisar University of Health Sciences Faculty of Dentistry, Afyonkarahisar, Türkiye
Received: 13 April 2024
Revised: 16 April 2024
Accepted: 16 April 2024
Published: 16 April 2024
ABSTRACT
| This study aimed to utilise borosilicate glass waste to produce dental ceramics. Commercially available borosilicate glass was crushed, and ground, and five different recipes were prepared by adding 3%, 6%, 9%, 12% and 15% by weight of zirconium oxide containing yttrium. The samples were subjected to fritting after melting at temperatures between 1450-1500°C, and after the powder mixtures, which were again crushed and ground, were condensed by layering or pressing methods and then sintered at 925°C. Based on the results, the sample with a 6% zirconium oxide additive, condensed using the pressing method, demonstrated the highest flexural strength. On the other hand, the group with a 15% zirconium oxide additive, prepared using the same technique, exhibited the lowest strength value. The sample prepared by the pressing method with 3% zirconia additive demonstrated the highest light transmittance. The sample prepared using the same process with 12% zirconia additive showed the lowest light transmittance. In conclusion, the light transmittance and colour properties of the samples obtained have values similar to those of dental ceramics. This experimentally prepared material can be used in dental restorations supported by a substructure when evaluated in terms of flexural strength. |
Keywords:
Dental ceramics, zirconium oxide, borosilicate glass.
Cite as: Akpınar S, Işisağ Ö. Evaluating the Manufacturability of Dental Ceramics from Borosilicate Glass Waste: A Pilot Study. Acta Med Eur. 2024;6(3):6-11. doi: 10.5281/zenodo.10980369
INTRODUCTION
Glass-ceramic composites are materials initially processed as glass and converted into glass-ceramic composites to improve the properties of ceramics. In other words, glass-ceramics are polycrystalline materials produced by controlled crystallisation and have much higher mechanical strength and lower coefficient of thermal expansion than glass (1,2). Glass-ceramics are often used in prosthetic treatments because of their high durability, resistance to wear in the oral environment, and natural tooth appearance (3). Glass matrix ceramics used in dental restorations are classified as feldspathic, glass infiltrated, and synthetic (4). The traditional type of dental ceramic is feldspathic ceramics that consist of feldspar (KAlSi3O8), quartz (SiO2) and kaolin (Al2O3-2SiO2-2H2O) (5). This material mimics natural tooth structure with high transparency and is layered onto metal, alumina or zirconia cores for prosthetic treatments (6).
Borosilicate glasses, produced by adding alkali to silica and boron oxide, are a widely used family of glasses, mainly because of their low coefficient of thermal expansion and high resistance to chemical attack (7). SiO2 and B2O3, the significant components of borosilicate glass, increase the transparency and chemical resistance of the glass (8). This property of the compounds has led researchers to investigate the optical and mechanical effects of B2O3 addition on dental materials. Yoshimura et al. (9) concluded that in dental ceramic compositions prepared with the addition of boron oxide, the light transmission of the final product was better than in ceramic alumina due to the excellent infiltration of boron oxide into the alumina and the filling of the porous structures inside, thanks to the reduction in the viscosity of the glass structure. In their study, Höland et al. (10) reported that adding boron oxide can make ceramics translucent to a degree comparable to natural teeth.
Nanomaterials exhibit superior properties compared to conventional materials, improving both the optical and mechanical properties of materials. Zirconia nanoparticles exhibit desirable properties such as high hardness, biocompatibility, and melting point, and they are used to improve the mechanical properties of dental materials (11,12).
New resource extraction methods have been developed and must be further implemented to derive more value from natural resources. Increased recycling of materials positively impacts the environment by reducing emissions and improving the sustainability of raw material usage (13). This pilot study aims to investigate the recycling of borosilicate glass waste, which contains about 13% boron compounds, for producing dental ceramics with high boron content. The idea for the research originated from the fact that borosilicate glass contains compounds similar to those of traditional feldspathic ceramics. It was thought that dental ceramics could be produced competitively with commercial products by adding a reinforcing element with high mechanical strength, such as zirconium oxide, to borosilicate glass waste. The research aims to make dental ceramics from borosilicate glass waste by recycling and transforming it into a valuable eco-product with environmental and economic benefits.
METHODS
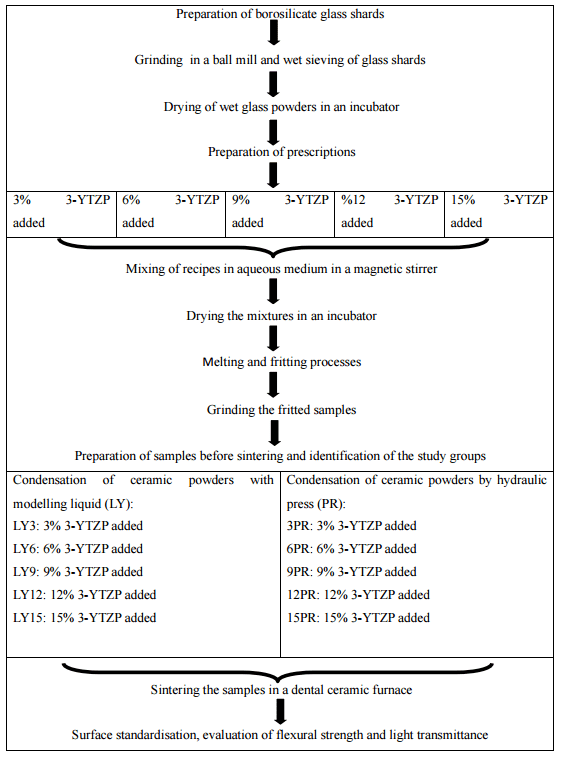
The materials used in the study are listed in Table 1. The flow chart of the research is shown in Table 2. This experimental study used a hammer to break commercially available borosilicate glasses into small pieces. During the breaking process, the hammer was wrapped in a thick towel to prevent the metal powders in the hammer from contaminating the glass fragments. The borosilicate glass shards that had been reduced to small pieces were added to the ball mill container, taking into account the volume of the ball mill container, and ground with alumina balls for 30 minutes. The glass powders removed from the mill were wet-sieved through 100-micron sieves. The glass powders remaining on the sieve were dried in an oven at 100 °C for 24 hours, ground in a ball mill for 30 minutes, and dried with the same protocol. Five different recipes were prepared by adding 3% (3), 6% (6), 9% (9), 12% (12) and 15%(15) w/w zirconia powder to the dried glass powders by weighing on a precision balance. In the recipe preparation process, after adding zirconium to the glass powders in the specified proportions, they were mixed in an aqueous medium with a magnetic stirrer for 30 minutes, and the mixed samples were dried in an oven at 100 °C for 24 hours. The dried samples were melted between 1450-1500°C, and the melted samples were subjected to a fritting process. After fritting, the samples were again crushed using a towel-wrapped hammer and ground in a ball mill for 30 minutes. All recipe groups were then divided into two sub-groups (condensed by layering (LY3, LY6, LY9, LY12, LY15) or pressing (PR3, PR6, PR9, PR12, PR15) methods), with the glass powders in the LY group mixed with dental modelling liquid. To ensure standardisation of the samples belonging to this group, the amounts of powder and modelling liquid were prepared in the same ratio in all recipe groups using a scaled spoon and dropper (2 scales of powder, ten drops of liquid). The powders in the PR group were pressurised to 100 bar in a hydraulic press in the dry state. All samples were sintered at 925°C in a dental ceramic furnace in standard moulds with a diameter of 14x4x2 mm for flexural strength and 10 mm and 2 mm thickness for light transmission. To standardise the surfaces of all specimens after sintering, the specimens to be evaluated for flexural strength were ground with #400, #600 and #800 silicon carbide papers and the specimens to be evaluated for light transmittance were ground with #400, #600, #800, #1000, #1200 and #1500 silicon carbide papers.
Table 1. Materials used in the study.
| Material | Brand, Manufacturer |
| Borosilicate glass | Paşabahçe Borcam, Paşabahçe, İstanbul, Turkey |
| Zirconium dioxide stabilised with 3 mol % yttrium | Yttria -Zirconia, Nanografi, Ankara, Turkey |
| Feldspathic dental porcelain powder | G-ceram, İzmir, Turkey |
| Modelling liquid | Çoşkan Dental, Turkey |
The flexural strength of the standardised specimens was assessed using a three-point flexure test in a universal testing machine, and the light transmittance was evaluated using a digital spectrophotometer. Translucency was measured using the translucency parameter (TP). The transmittance was obtained by calculating the colour difference of the sample on black and white backgrounds using the formula TP = [(LB – LW)2 + (aB – aW)2 + (bB – bW)2]½. In this formula, the values L, a and b are the colour parameters recorded on the spectrophotometer for each sample. LB, aB and bB are the L, a and b parameters of the samples measured on a black background, and LW, aW, and bW are the L, a and b parameters of the samples measured on a white background. TP is the translucency parameter. “When the TP value increases, the material becomes more translucent.” Flexural strength was calculated using equation 3Pl/2wh2. Where P is the value of the load at the moment of failure in Newtons; l is the distance between the supports; w is the width of the specimen; h is the height of the specimen. In addition, a sample of feldspathic ceramic, often used in prosthetic treatments, was prepared to compare light transmission, and TP was compared with all groups.
The numerical values of the specimens’ light transmittance were compared within each other and with the control group, and the flexural strengths were analysed with mean and standard deviation values. In addition, the values obtained from the experiment were compared with those of ceramic and ceramic-like materials used in existing dental treatments.
Table 2. Flow diagram of the study.
RESULTS AND DISCUSSION
Table 3 displays a detailed analysis of the flexural strengths of the samples, along with their mean and standard deviation values. The table also provides the samples’ TP values. After analysing the results, it was discovered that the PR6 group had the highest flexural strength, while the PR15 group had the lowest. Figures 1a and 1b compare the light transmittance of ceramics produced by different condensation techniques and made from various formulations. Additionally, Figure 1c shows a visual comparison of the light transmission of the sample with the highest translucency parameter when compared to a commercial feldspathic ceramic. The PR3 group had the highest TP value, while the PR12 group had the lowest, indicating lower transparency. When the flexural strengths of all prescription groups were evaluated, there was no statistically significant difference between the groups (p>0.05).
Table 3. Flexural strength values and the translucency parameters of the samples.
| Groups | Flexural strength (n=3) (MPa) | Translucency Parameter (n=1) |
| CTR | NA | 14.06 |
| LY3 | 83.81±16.71A | 12.47 |
| LY6 | 69.95±11.08A | 13.55 |
| LY9 | 59.21±12.54A | 7.41 |
| LY12 | 70.46±12.44A | 5.75 |
| LY15 | 50.17±10.92A | 2.95 |
| PR3 | 62.65±12.06A | 15.07 |
| PR6 | 91.98±0.69A | 13.92 |
| PR9 | 69.40±21.93A | 10.34 |
| PR12 | 70.64±5.55A | 0.48 |
| PR15 | 49.40±10.92A | 1.25 |
Different letters written with superscripts in the same column indicate statistical difference (p<0.05). CTR: Control, NA: Not applicable.
In this study, borosilicate glass waste was ground and zirconia was added to these ground powders at specific weight ratios. According to the results of the study, the samples produced with 3% and 6% zirconium oxide additions are similar to dental ceramics used in routine treatment in terms of light transmission and colour. Considering the results of the study, it can be concluded that this experimentally formed material has a significantly lower flexural strength than dental ceramics applied without any substrate requirement; on the other hand, especially the recipes with 3% and 6% zirconium oxide addition have similar values to the flexural strength of dental ceramics coated on the substrate. A study evaluating the flexural strength of veneering ceramics concluded that the flexural strength of different ceramics varied between 61.6 MPa and 120.8 MPa (14). In another study, this value was found to be 69.8 and 65.5 MPa for two different veneering ceramics (15). Another study reported that the flexural strength of 13 different veneering ceramics ranged from 77.8 MPa to 149.4 MPa (16). From this point of view, this ceramic material can be used in prosthetic treatments supported by metal or zirconium substructures as long as it has appropriate mechanical and biological parameters (17–19).



Figure 1. Figures 1a and b. Visual comparison of the light transmission of ceramics made from different formulations and produced by different condensation techniques. Figure 1c. Visual comparison of the light transmission of the sample with the highest translucency parameter with a commercial feldspathic ceramic.
The present study compared the light transmission (TP) parameter with feldspathic ceramics used in routine treatment. The reason for using feldspathic ceramics is that the light transmittance is clinically acceptable (20) and to evaluate the achievability of the same property in experimentally prepared glass ceramics. The light transmittance values of the samples with 3% and 6% zirconia additions were very close to those of the feldspathic ceramics, such that the sample belonging to the 3PR group had a higher TP value than the feldspathic ceramic. The ceramic samples produced in this context are clinically acceptable regarding light transmission. The samples with high zirconia content had lower TP values due to the opaque structure of zirconia, hindering light transmission.
The formulations prepared in the study were melted at temperatures between 1450-1500 °C. The low strength may be because the zirconia particles are not completely melted at this temperature range, and the mixture is not homogeneously distributed. Another finding supporting this situation is that the higher zirconia formulations had lower flexural strength than the others. Although strength is expected to increase in the groups where a high-strength material such as zirconium is added at a higher rate (groups with 12% and 15% added), the lower strength values may be because the melting temperature of the zirconium in the powder mixture is not high enough. The zirconium and glass powders are not homogeneously distributed.
The sintering temperature is an important parameter affecting zirconia particles’ porosity rate and growth. It can also affect the strength and durability of zirconia (21). In this study, the sintering temperature was 925°C. However, the low flexural strength of zirconium-containing samples suggests that this temperature is not sufficient.
Rough or irregular ceramic surfaces can cause stress concentration and initiate crack propagation, leading to several failures in ceramic restorations (21). A study investigating the effect of hydrofluoric acid roughening time on surface roughness and glass matrix ceramics’ flexural strength decreased as surface roughness increased (22). In the current study, the surfaces of the specimens to be tested for mechanical strength were standardised using abrasives with grits of #400, #600 and #800. Another reason for the low flexural strength found in the study results may be that the abrasives used to standardise the surface of the specimens did not produce sufficient roughness.
This study has limitations, including a small sample size and a limited range of zirconium ratios added to the borosilicate powder. Different sintering times and temperatures were not evaluated, and only bending strength and translucency parameters were analysed. Further research should examine other factors, such as fracture toughness, hardness, and thermal conductivity, and determine sintering times and temperatures through thermal analyses. Structural evaluations can be carried out using SEM and EDX analyses.
CONCLUSION
As a result, the samples’ light transmission and colour properties have similar values to those of dental ceramics. This experimentally produced material can be used in dental restorations supported by a substructure when evaluated in terms of flexural strength. This study can guide the production of dental ceramics with acceptable optical and mechanical properties by recycling borosilicate glass waste.
Author contributions
Süleyman Akpınar: Conceptualization; formal analysis; investigation; project administration; resources; supervision; writing—original draft.
Özer İşisağ: Investigation;writing—original draft
Acknowledgement
We wish to thank Afyon Kocatepe University Scientific Research Projects Unit.
Funding
This research was funded by the Research Fund of the Afyon Kocatepe University Scientific Research Projects Unit under grant number 21.FEN.BİL.42.
Conflict of interest
The authors do not have any financial interest in the companies whose materials are included in this article.
ORCIDs:
SA: 0000-0002-7959-3464
OI: 0000-0002-2042-958X
REFERENCES
- Omar AA, El-Shennawi AWA, El-Ghannam AR. Thermal expansion of Li2O-ZnO-Al2O3-SiO2 glasses and corresponding glass-ceramics. J Mater Sci. 1991;26(22):6049–6056. doi:10.1007/BF01113882
- Rafea OAS, Salem ANM, Badr IHA. Preparation and characterization of high chemical durability and low thermal expansion borosilicate glass-ceramic composites by recycling of borosilicate glass. Egypt J Chem. 2021;64(4): 2193-2199. doi:10.21608/EJCHEM.2021.54579.3139
- Höland W, Rheinberger V, Apel E, et al. Clinical applications of glass-ceramics in dentistry. J Mater Sci Mater Med. 2006;17(11):1037-1042. doi:10.1007/s10856-006-0441-y
- Gracis S, Thompson VP, Ferencz JL, Silva NR, Bonfante EA. A new classification system for all-ceramic and ceramic-like restorative materials. Int J Prosthodont. 2015;28(3):227-235. doi:10.11607/ijp.4244
- Bajraktarova-Valjakova E, Korunoska-Stevkovska V, Kapusevska B, Gigovski N, Bajraktarova-Misevska C, Grozdanov A. Contemporary Dental Ceramic Materials, A Review: Chemical Composition, Physical and Mechanical Properties, Indications for Use. Open Access Maced J Med Sci. 2018;6(9):1742-1755. doi:10.3889/oamjms.2018.378
- McLaren EA, LeSage B. Feldspathic veneers: what are their indications?. Compend Contin Educ Dent. 2011;32(3):44-49.
- Lima MM, Monteiro R. Characterisation and thermal behaviour of a borosilicate glass. Thermochim Acta. 2001;373(1-2):69-74. doi:10.1016/S0040-6031(01)00456-7
- Zinina EM, Savinkov VI, Klimenko NN, et al. Influence of Boron Oxide on the Technological Properties of Strontium Aluminosilicate Glasses for Dentistry. Glass and Ceramics (English translation of Steklo i Keramika). 2023;79(11-12): 439–442. doi:10.1007/s10717-023-00528-2
- Yoshimura HN, Chimanski A, Cesar PF. Systematic approach to preparing ceramic-glass composites with high translucency for dental restorations. Dent Mater. 2015;31(10):1188-1197. doi:10.1016/j.dental.2015.06.015
- Holand W, Frank M, Rheınberger V. Influence of small quantities of boron oxide additives on the microstructure and optical properties of dental glass-ceramics. In: Borate glasses, crystals & melts. ; 1997:332-339.
- Ahmed MA, Ebrahim MI. Effect of Zirconium Oxide Nano-Fillers Addition on the Flexural Strength, Fracture Toughness, and Hardness of Heat-Polymerized Acrylic Resin. World Journal of Nano Science and Engineering. 2014;04(02):50-57. doi:10.4236/wjnse.2014.42008
- Gad MM, Abualsaud R, Rahoma A, Al-Thobity AM, Al-Abidi KS, Akhtar S. Effect of zirconium oxide nanoparticles addition on the optical and tensile properties of polymethyl methacrylate denture base material. Int J Nanomedicine. 2018;13:283-292. doi:10.2147/IJN.S152571
- Ervasti I, Miranda R, Kauranen I. A global, comprehensive review of literature related to paper recycling: A pressing need for a uniform system of terms and definitions. Waste Manag. 2016;48:64-71. doi:10.1016/j.wasman.2015.11.020
- Tang X, Nakamura T, Usami H, Wakabayashi K, Yatani H. Effects of multiple firings on the mechanical properties and microstructure of veneering ceramics for zirconia frameworks. J Dent. 2012;40(5):372-380. doi:10.1016/j.jdent.2012.01.014
- Borba M, de Araújo MD, de Lima E, et al. Flexural strength and failure modes of layered ceramic structures. Dent Mater. 2011;27(12):1259-1266. doi:10.1016/j.dental.2011.09.008
- Fischer J, Stawarczyk B, Hämmerle CHF. Flexural strength of veneering ceramics for zirconia. J Dent. 2008;36(5). doi:10.1016/j.jdent.2008.01.017
- IPS E.max® Ceram scientific document. Accessed February 29, 2024. https://ivodent.hu/__docs/770_9bdf4c16113cbf649ec4578d581cd9f6.pdf
- Vita Suprınıty® PC Technical and Scientific Documentation. Accessed February 29, 2024. https://www.vita-zahnfabrik.com/en/VITA-SUPRINITY-PC-44049.html
- Attar EA, Aldharrab A, Ajaj R. Flexural Strength Properties of Five Different Monolithic Computer-Aided Design/Computer-Aided Manufacturing Ceramic Materials: An In Vitro Study. Cureus. 2023;15(3):e36958. doi:10.7759/cureus.36958
- Chitsaz F, Ghodsi S, Harehdasht SA, Goodarzi B, Zeighami S. Evaluation of the colour and translucency parameter of conventional and Computer-aided design and computer-aided manufacturing (CAD-CAM) feldspathic porcelains after staining and laser-assisted bleaching. J Conserv Dent. 2021;24(6):628-633. doi:10.4103/jcd.jcd_273_21
- Fischer H, Schäfer M, Marx R. Effect of surface roughness on flexural strength of veneer ceramics. J Dent Res. 2003;82(12):972-975. doi:10.1177/154405910308201207
- Keshmiri N, Alaghehmand H, Mokhtarpour F. Effect of Hydrofluoric Acid Surface Treatments on Surface Roughness and Three-Point Flexural Strength of Suprinity Ceramic. Front Dent. 2020;17(22):1-7. doi:10.18502/fid.v17i22.4316
