Yasuhiro Horiuchi 1
1 Division of Dermatology, Tsuruse Orthopedic Clinic, Saitama, Japan.
Received: 3 June 2024
Revised: 19 June 2024
Accepted: 19 Jun 2024
Published: 19 Jun 2024
Corresponding author:
Yasuhiro Horiuchi.
Division of Dermatology, Tsuruse Orthopedic Clinic, 201-11 Fujikubo, Miyoshi, 354-0041 Saitama, Japan.
tshoriuchi15@gmail.com
ORCID: 0000-0002-6805-7084
Cite as:
Horiuchi Y. Consideration of Ineffectiveness of Oral Care in Alzheimer’s Disease and Type 2 Diabetes. Acta Med Eur. 2024;6(3):77-78. doi: 10.5281/zenodo.12152386
doi: 10.5281/zenodo.12197694
ABSTRACT
| Recently, evidence has suggested that periodontal disease, such as periodontitis, may be associated with other systemic diseases such as diabetes and Alzheimer’s disease. The pathogenesis of these systemic diseases caused by oral bacteria is very different from that of leukocyte-mediated inflammation in palmoplantar pustulosis, but in Alzheimer’s disease, there is accumulation of bacterial components and immune reactants in the brain. Even if these systemic diseases are caused by oral bacteria, it is assumed that the pathogenic mechanism differs, depending on the individual disease. It is necessary to reconsider the importance and difficulty of oral care for the treatment of systemic diseases caused by oral bacteria. |
Keywords:
Oral bacteria, systemic diseases, Alzheimer’s disease, type 2 diabetes, palmoplantar pustulosis
Dear Editor,
Recently, evidence has suggested that periodontal disease, such as periodontitis, may be associated with several systemic diseases (1) (Figure 1) such as Alzheimer’s disease (AzD) (2) and type 2 diabetes. A recent study (3) reported that palmoplantar pustulosis (PPP), a unique chronic inflammatory disease characterized by pustules on the palms and soles (3) (Figure 1), may be caused by oral bacteria, and can be cured with ozonated water oral rinse (3). Periodontal bacteria, which colonize in the mouth (1,2,3), can no longer be overlooked as indigenous bacteria. Here, the author discusses the relationship between periodontal bacteria and systemic diseases.
Alzheimer’s disease is mainly caused by the accumulation of amyloid in the brain (2). Moreover, it has been suggested that oral bacteria are involved in the occurrence of PPP due to leukocyte-mediated inflammation (3). So far, the pathogenesis of these systemic diseases caused by oral bacteria is very different from that of leukocyte-mediated inflammation in PPP (3), but in AzD (2), accumulation of bacterial components and immune reactants occurs. Therefore, in AzD, there is a possibility that oral sterilization will not be effective because the accumulated complexes cannot be removed even by eradicating causative bacteria by ozone water oral rinsing.
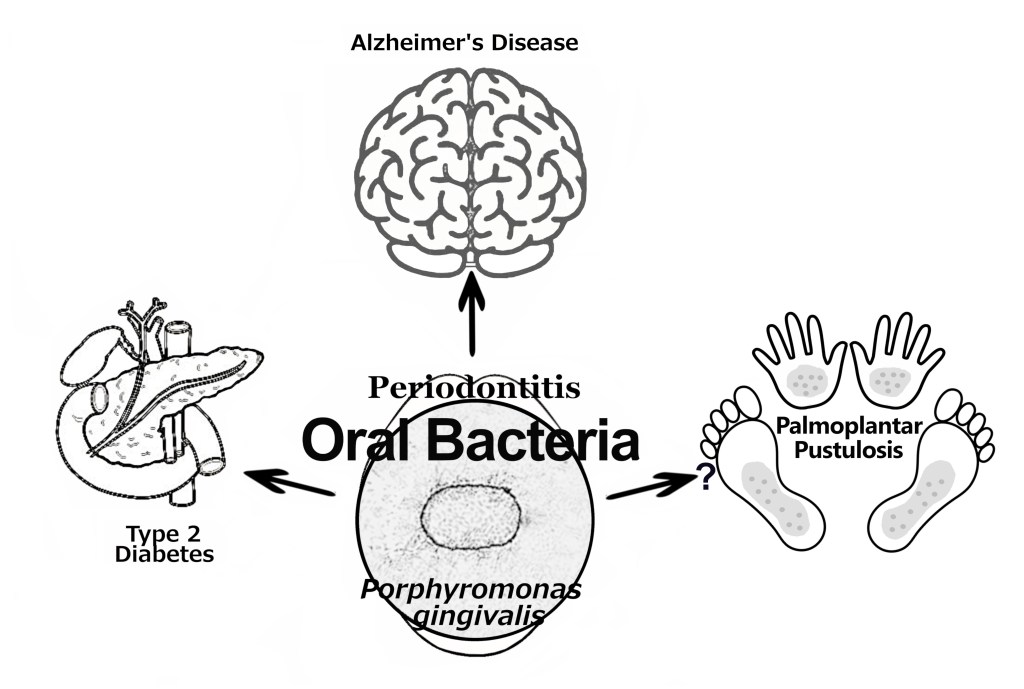
Figure 1. Representative illustration of systemic diseases, periodontal diseases and oral bacteria.
The author encountered two patients with systemic diseases associated with oral bacteria. The first patient was a 92-year-old woman with severe Alzheimer’s dementia who was unable to recognize herself. The second case involved a 56-year-old obese man with type 2 diabetes (weight: 95 kg; HbA1c level: 8–9%). In both cases, an oral ozone water rinse was administered. For the patient with Alzheimer’s, the procedure was carried out with the family’s consent, while for the patient with diabetes, it was performed at his own request.
No improvement was observed in the symptoms of both AzD and diabetes even after cleaning treatment for a period of 4 months. In diabetes, the immune complex under oral bacteria influence would lead to the progression of the disease, leading to disruption of islet cell functions in the pancreas. Even if oral bacteria possibly responsible for diabetes are sterilized with ozone water, the impaired pancreatic islet function cannot be recovered and the symptoms may not improve, although the possibility of the involvement of intestinal bacteria has not been completely denied. It has been pointed out that the treatment of periodontitis is associated with reduced HbA1c level of approximately 0.4% only (4). It has been reported that component substances of Porphyromonas gingivalis (P. gingivalis) (Figure 1) can contribute to the development of AzD (2), but P. gingivalis has walls with an oxidation-resistant structure (5). Even if P. gingivalis is an oxidation-tolerant bacterium, precautions should be taken before AzD and type 2 diabetes onset.
In conclusion, it is assumed that the immune response to the components of causative bacteria differ individually, as the pathogenic mechanism differs depending on the individual disease. It is necessary to reconsider the importance and difficulty of oral care for the treatment of systemic diseases caused by oral bacteria.
Ethics and consent
This institution completed a clinical study of palmoplantar pustulosis using nano-ozone water under the approval of the Japan Medical Association Ethics Committee. However, Alzheimer’s disease and type 2 diabetes cannot be obtained by accumulating cases and obtaining approval from an ethical review. The patients’ consent to ozone oral rinse was obtained from her daughter of a 92-year-old patient, and a 56-year-old patient in verbally. The ozone nanobubble water oral rinse was performed with the patient’s family member or patient own discretion and volition, and in the accordance with the Helsinki Declaration.
Acknowledgment
The author thanks Editage for English language editing.
Conflict of interest
The author does not have any conflict of interests.
Funding
This article received no financial support.
Author contributions
Yasuhiro Horiuchi: Conceptualization; formal analysis; investigation; project administration; resources; supervision; writing—original draft.
Data confidentiality
On request, all data and study protocol can be made available.
CC BY Licence
This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/)
REFERENCES
- Bourgeois D, Inquimbert C, Ottolenghi L, Carrouel F. Periodontal pathogens as risk factors of cardiovascular diseases, diabetes, rheumatoid arthritis, cancer, and chronic obstructive pulmonary disease-Is there cause for consideration? Microorganisms. 2019;7(10):424. doi: 10.3390/microorganisms7100424
- Matsushita K, Yamada-Furukawa M, Shikama Y. Periodontal disease and periodontal disease-related bacteria involved in the pathogenesis of Alzheimer’s disease. J Inflamm Res. 2020; 13:275-283.
- Horiuchi Y. Palmoplantar pustulosis treated with oral rinse using ozone nanobubble water: A case series. Dermatol Ther. 2020; 33(6):e13924. doi: 10.1111/dth.13924
- Preshaw PM, Alba AL, Herrera D, Jepsen S, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21-31. doi: 10.1007/s00125-011-2342-y
- Henry LG, McKenzie RME, Robles A, Fletcher HM. Oxidative stress resistance in Porphyromonas gingivalis. Future Microbiol. 2012;7(4):497-512. doi: 10.2217/fmb.12.17
