Neslihan Kurtul 1, Selami Eken 1
1 Department of Radiation Oncology, Kahramanmaras Sutcu Imam University Faculty of Medicine, Kahramanmaras, Turkey
Received: 14 June 2024
Revised: 26 June 2024
Accepted: 26 June 2024
Published: 26 June 2024
Corresponding author:
Selami Eken.
Department of Radiation Oncology, Kahramanmaras Sutcu Imam University Faculty of Medicine, Kahramanmaras, Turkey.
selamieken@ksu.edu.tr
ORCID: 0000-0001-9320-0391
Cite as:
Kurtul N, Eken S. Comparative Analysis of Secondary Cancer Risks in Breast Cancer Radiotherapy: Evaluating Low Dose Volumes and Monitor Units in IMRT and VMAT Techniques. Acta Med Eur. 2024;6(3):95-100. doi: 10.5281/zenodo.12543200
doi: 10.5281/zenodo.12543200
ABSTRACT
| Development of secondary cancer due to radiotherapy can be associated with alot of factors. It is believed that low dose volume and and monitor unit (MU) values in radiation therapy plans for breast radiation therapy are associated with this development. This study aimed to evaluate and compare the intensity modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) techniques for breast radiotherapy in terms of secondary cancers. The VMAT and IMRT plans of 11 breast cancer patients were evaluated. MU and low dose volume (5, 10 and 20 Gray) of each patient in both VMAT and IMRT plans were calculated and compared. The differences between the two techniques were examined. The calculated VMAT-MU (mean MU: 1104±158) was found to be lower than IMRT-MU (mean MU: 1459±325). The mean low dose volumes (V5, V10, V20) of VMAT and IMRT were compared. VMAT – mean low dose volume compared to IMRT, but the difference found no statistically significant. In conclusion, due to the low number of MU in breast cancer radiation therapy, the VMAT technique may be preferred instead of the IMRT technique. |
Keywords:
Monitor unit, low dose volume, radiotherapy.
INTRODUCTION
Cancer is a disease that develop as a result of uncontrolled proliferation and growth of cells in any organ or tissue of the body. Breast cancer is the most common type of cancer among women and the breast cancer rate is 24% of cancers worldwide (1). In addition, the risk of developing breast cancer during a woman’s lifetime is in the range of 10-12% (2). With the widespread use of cancer screening methods, an increase in early diagnosis and treatment success of breast cancer has also been achieved with developing new treatment techniques. The increase in treatment success has supported the further development of existing techniques. In some studies, it has been observed that radiotherapy, one of these techniques, reduces local-regional recurrence, increases disease-free and overall survival (3-5). Breast radiotherapy technique shows personal differences due to the anatomical structure and diversity of the breast area. In accordance with the general purpose of radiotherapy, it should be remembered that critical organs (such as the lung, heart and other breast) should receive as low as dose possible when irradiate the target area homogeneously.
In recent years, with new developed treatment devices and planning techniques, normal tissues and critical organs dose can be reduced, and it is possible to give high doses for tumor. Standard treatment technique has not yet been recommended for breast radiotherapy. Intensity modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) treatment techniques are used. In IMRT technique, the intensity of the radiation beam is changed by a continuous moving multileaf collimator (MLC). Adjusting the beam intensity within each fixed angle treatment field helps to create more conformal dose distributions within the target volume. One or more arcs can be used in the VMAT treatment technique. The gantry rotation speed, dose rate and MLC leaf positions change simultaneously for provide conformal dose distribution (6). When they compared with 3D-conformal radiotherapy (3DCRT), an older technique than these techniques, it has been shown that the dose uniformity and conformality of the target volume increases with the help of IMRT and VMAT techniques in the radiotherapy of many different anatomical regions, and at the same time the radiation doses received by normal tissues decrease (7-10). This decrease reduces radiation-induced harm to the surrounding organs and tissues. Because radiation-induced damage is associated with the volume of radiation exposure of an organ or tissue and the radiation dose. For this reason, normal tissues should be protected from radiation as much as possible during radiation therapy (11,12). Radiation therapy-related side effects are evaluated in two ways as functional (acute, chronic) and oncogenesis. These side effects, which caused by radiation therapy, are factors that limit the total radiation dose (13). In addition, the probability and severity of toxicity that may develop in normal tissue in the irradiated area also depends on factors related to the type of radiation, total dose, fraction dose, irradiated area and dose homogenity.
With the help of new treatment techniques, the survival of cancer patients continues to increase. But this result can also lead to an increase in the incidence of secondary cancer in the treated areas. One of the most serious late side effects of radiation therapy are radiation-related secondary cancers. Changes in supressor genes can lead to the expression of oncogenes. With sublethal damage, normal genes can turn into oncogenes (14). Suppression of the immune system may affect the development of cancer. It may take up to ten years for these effects to show (15). A higher incidence of secondary cancer was reported in patients received radiation therapy than in patients who didnt receive it. In addition in ongoing studies on secondary cancers, different results shared for different treatment sides. In addition, research is ongoing on whether variables (MLC, Monitor Unit-MU) related to the planning technique cause secondary cancer. MLC movement, number of MU and dose rate vary according to the planning technique. Monitor Unit is a different expression of the radiation dose required for radiotherapy. Monitor Unit calculated with different parameter. These parameters include field size, depth in tissue, wedge and dose distribution of each field. It has been estimated that doubled the MU increase (1.2) the risk of secondary cancer (16,17). In addition, increasing the number of MU extend the treatment time. As a result of this, the target moves more. This movement may cause irradiation of a larger volume of healthy tissue (18,19).
Wide irradiation volume can create the wide low dose radiation volume. Angiogenesis, which can occur as a result of low doses, can cause extra tumor growth and new metastases (20,21). For this reason, there is a lot of research on the relationship between the low dose region and the treatment technique. The risk of secondary cancer may increase due to increased low dose volumes when intensitiy-modulated radiotherapy techniques are used (22,23). Knapp et al. found the low dose volume in IMRT to be higher than in other techniques (24). However, Lii et al. found the low dose volume in the VMAT technique to be lower than in other techniques. In addition, when studies in breast cancer radiation therapy were also examined, Mishra et al. and Adeyene et al. measured higher low dose volumes in VMAT plans (25,26). It was commented that VMAT alone does not offer any significant benefit. However, Canbolat et al. measured it lower than IMRT (27). Therefore, not only MU but also the size of the low dose volume is an important criterion in choosing treatment plan technique.
In this study, it was aimed to compare the low dose volume and Monitor Unit associated with IMRT and VMAT techniques used in breast cancer radiotherapy in terms of secondary cancer risk.
METHODS
Radiation therapy plans of 11 patients diagnosed with right breast cancer who were treated at the our department in 2024 were used. All patients underwent a mastectomy followed by radiotherapy. Axilla (AX), superclavicular area (SCF) and chest wall areas were in the treatment field. Two different radiotherapy plans were designed for each patient using both IMRT and VMAT treatment techniques. Gross tumor volume (GTV), clinical tumor volume (CTVtm) and lymph nodes (CTV lymph nodes) and organs at risk were identified and contoured with the Radiation Therapy Oncology Group Atlas (RTOG) for treatment planning. The treatment volume (PTV) were contoured under the guidance of RTOG Atlas. Treatment plans were designed to deliver 50 Gy in daily fractions of 2 Gy to AX, SCF and chest wall.
Treatment planning
IMRT technique
This technique requires multiple fixed-angle radiation beams. The gantry don’t move around the patient. Multiple fields used for treatment planning. Dose rate is variable and multileaf collimators are in continuous movement for provide to conform dose distribution.
The IMRT plans were designed with the Eclipse 13.0 (Varian Medical Systems, Inc) treatment planning system. When preparing the treatment plan, 6 MV X-ray and Beam Eye View (BEV) were used to decide on the treatment fields. In such away that the fields do not see each other directly, 0°, 33°, 60°, 196°, 220°, 263°, 314° field angles and collimator angle of 0° were used. A 5 mm thick bolus was used to cover the chest wall. All fields were opened up to the total of the PTV volumes (Figure 1). The dose rate was determined as 400MU/min.
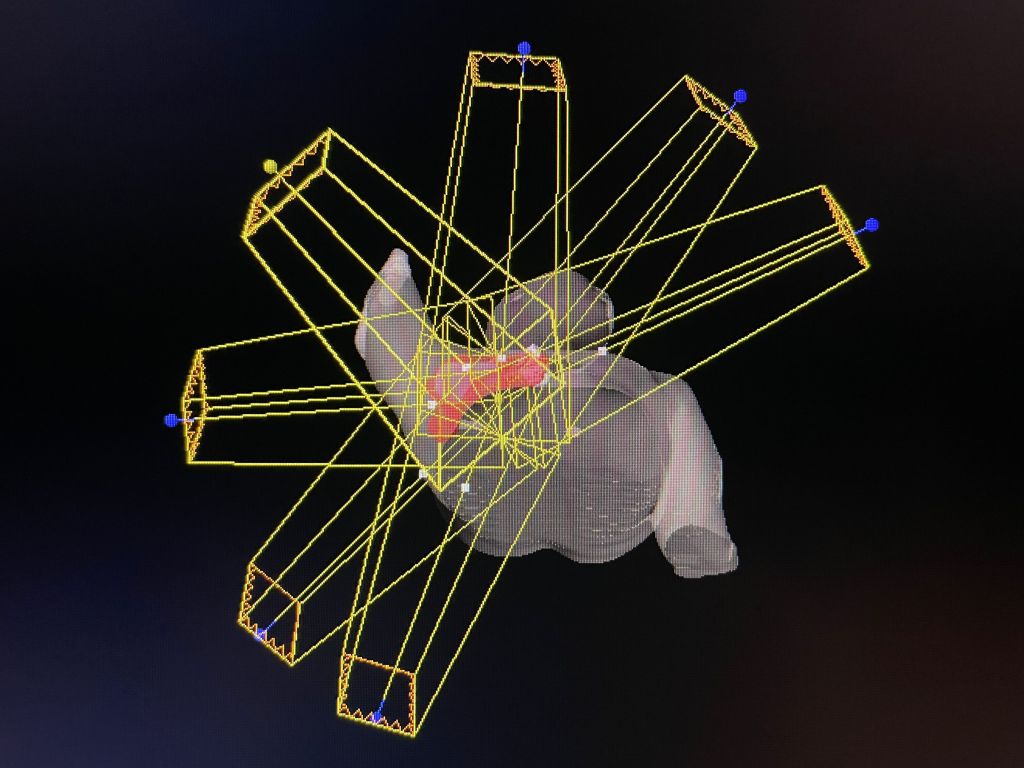
Figure 1. Gantry angles for IMRT.
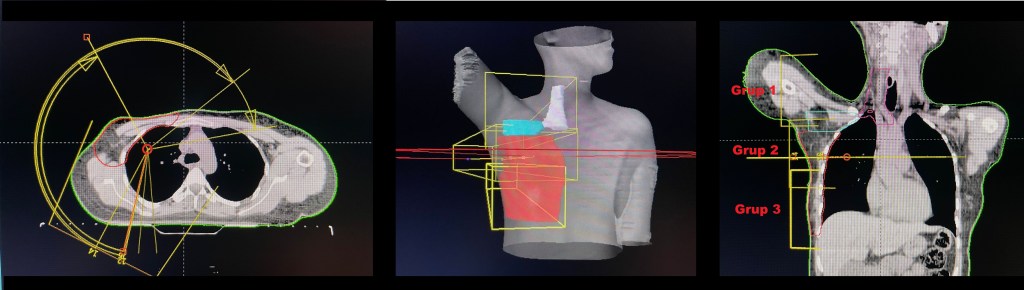
Figure 2. Gantry angles for VMAT.
VMAT technique
The gantry moves continuously around the patient in VMAT technique. Single or multiple arcs can be choose. Dose rate is variable and multileaf collimators are in continuous movement for provide to conform dose distribution. VMAT plans were designed with the Eclipse 13.0 treatment planning system. The single isocenter method was used.
VMAT plans were designed with of 8 arc fields (4 clockwise (CW) and 4 counterclockwise (CCW)). Grup-1 fields (Start-Stop); 192°-61° CW, 61°-192° CW. Grup-2 field (Start-Stop); 210°-80° CW, 80°-210° CCW. Grup-3 field (Start-Stop); 64°-305°, 300°-190° CCW, 190°-300°, 305°-64° CW and collimator angle was set to 0°. The upper and/or lower jaws of the fields were overlapped (min. 1cm) (Figure 2). A 5 mm thick bolus was used to cover the chest wall. The dose rate was determined as 400MU/min.
Dose-volume histograms (DVH) of the PTV and the OARs were calculated to compare the dosimetric quality of the VMAT and IMRT plans. Plan evaluation rules; ≥ 5% of PTV receiving 110%≥ of the prescribed dose, ≥ 95% of PTV receiving 95%≥ of the prescribed dose, None of the PTV volume should receive 115%≥ of the prescribed dose.
Heart, ipsilateral lung, contralateral breast and contralateral lung were accepted as the organ at risk. Critical organ dose criteria recommended by Emami have taken into account for evaluation of critical organs. Plans that meet all the criteria have been taken into consideration.
VMAT and IMRT plans of the same patient were compared with each other. Different number of MU for each field is calculated by a treatment planning system for IMRT and VMAT plans. Therefore, the total number of MU was used for comparison. The volume (cm3) of 5, 10 and 20 Gray (V5-V10-V20) were measured to determine the low dose radiation volume of IMRT and VMAT plans. Volume / Body restrictions were not applied. The PTV volume was not cropped from the low dose regions.
RESULTS
Both VMAT and IMRT plans of 11 patients who treated in 2024 were evaluated in our clinic. The total MU in both VMAT and IMRT plans of the same patient was calculated (Figure 3).
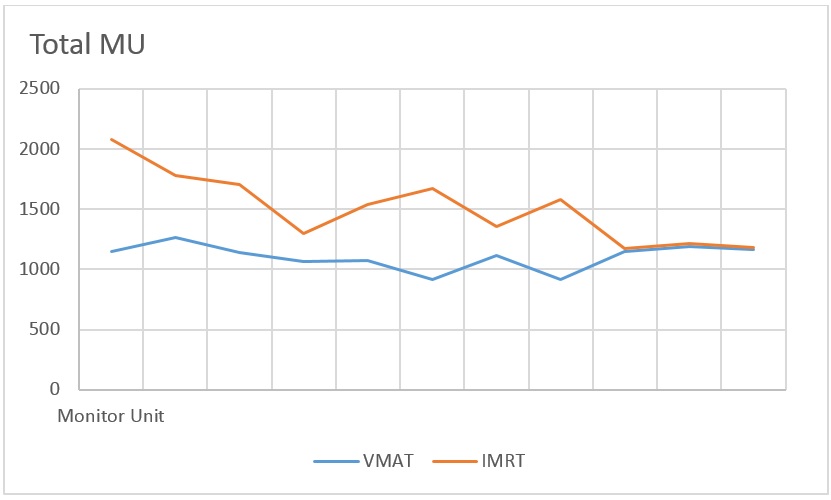
Figure 3. Total MU for VMAT and IMRT.
There was a significant difference between MU. The MU calculated of the VMAT plans was found to be smaller than the IMRT plans. VMAT-MU; min:714, max:1269, mean:1104±158. IMRT-MU; min:970, max:2082, mean:1459±325. For IMRT and VMAT techniques, mean MU are shown in Table 1. The difference found between the two methods are statistically significant (p<0.05).
Table 1. Mean MU and Mean V5, V10, V20 of VMAT and IMRT.
| VMAT | IMRT | p | |
| MU | 1104±182 | 1459±325 | <0.05 |
| V5 (cm3) | 9340±2291 | 9566±2457 | 0.105 |
| V10 (cm3) | 5618±1651 | 5867±1748 | 0.112 |
| V20 (cm3) | 4012±1201 | 4273±1355 | 0.150 |
VMAT: Volumetric modulated arc therapy, IMRT: Intensity modulated radiotherapy, MU: Monitor Unit.
The low dose radiation volumes (V5, V10, V20-cm3) in the VMAT and IMRT plans were determined (Figure 4,5,6). For IMRT and VMAT techniques, mean low-dose volume shown in Table 1. There was a difference between the mean v5, v10, v20 volumes of IMRT and VMAT techniques. However, this difference between the two techniques was not statistically significant. (p: 0.105,0.112,0.15).

Figure 4. V5 for VMAT and IMRT.

Figure 5. V10 for VMAT and IMRT.

Figure 6. V20 for VMAT and IMRT.
DISCUSSION
The aim of radiotherapy is protect the critical organs while covering the PTV as much as possible with treatment dose. To achieve this, we need innovative treatment techniques. Technological advances in radiotherapy have allowed the use of innovative intensity modulated planning techniques that not only increase tumor coverage in the treatment of breast cancer, but also protect the critical organs better than compared to traditional three-dimensional conformal radiotherapy (28-31). A lot of research done on treatment techniques. Some of these studies are related to both oar protection and PTV coverage. They showed that VMAT provides better target volume coverage, dose uniformity and organ at risk protection compared to the IMRT technique (32). In different studies, PTV coverage was found to be similar for IMRT and VMAT techniques (33-36). Some studies have been conducted on the risk of secondary cancer. Theoretical concerns have been raised that intensity-modulated radiotherapy techniques such as IMRT and VMAT potentially cause an increase in the risk of secondary cancer compared to 3D-CRT (37-39).
The risk of secondary cancer due to radiation therapy is become one of the important factors affecting the decision-making process for the technique to be applied in the treatment of cancer patients who will be treated with radiation therapy. Factors such as the volume and dose of the irradiated area, low radiation dose volume, irradiated organ, tissue type, radiation therapy technique used, age and family cancer history affect the development of secondary cancers related with radiation therapy. It is known that new techniques with more treatment fields lead to the risk of secondary cancer, as they increase the low-dose region. In some studies, it has been stated that secondary malignancies are related to low dose (<0.2 Gy). The risk of secondary cancer is especially pronounced in young patients. The relative risk is reported to be between 1.32 and 1.59 in women under the age of 45, and 1.01 in women over the age of 45 (40). It has also been reported that radiation-induced thyroid and breast cancers can be observed at doses as low as 100 mGy (41). Studies conducted for the lung region indicate that there may be a relation between a low dose and a relapse-free life. Due to these risks, it is desirable that the low dose volume should be as low as possible.
Although there is a difference between the low dose regions measured in the VMAT and IMRT plans of the same patient in our study, it is observed that this difference is very small (Figures 4, 5, 6). The total volumes of V5-V10-V20 (cm3) were found to be close to each other. From a patient-based perspective, the low dose volume did not make a significant difference in terms of VMAT or IMRT. There is no clear consensus in the literature about the low dose volume formed by the difference in planning technique. The studies examined have given different results from each other. In some of these studies, the low dose volume was found to be high in IMRT technique, while in others, the low dose region in VMAT technique was found to be high (24-26,42). This study shows the low dose volume can change with treatment technique. But this difference may be statistically non-significant. In addition, in our study, it was observed that the number of fields in the VMAT technique greater than the number of fields in the IMRT technique has no effect on the volume of the low dose region in our study.
There is a difference between IMRT and VMAT techniques. When the studies related to this difference are examined; it has been reported that a low MU reduces the risk of secondary cancer in studies related to MU (16,17). IMRT uses more fields and monitor units, which cause a higher whole-body exposure due to leakage radiation. An increase in the number of MUs is correlated with an increase in out-of-field radiation dose (43). When calculating the MU, while its value varies according to the parameters in the formula used, the effect of the result on the patient leads to the conclusion that the MU results should be evaluated from a different point of view. These and similar results lead to questioning not only the low dose region, but also the MU. In addition to low dose comparisons, the MU of both planning techniques were compared in our study.
In this study; It has been observed that there were higher MU in IMRT technique compared to VMAT technique (Figure 3). The mean MU was found to be 1104±158 in the VMAT method and the mean MU was found to be 1459±325 in the IMRT method. In all treatment plans, the MU in the VMAT plan was less than the MU value in the IMRT plan. These results are consistent with previous studies (25,27). The number of MU per Gray decreased in the VMAT technique. The effect of the previously mentioned MU on secondary cancer could further reduced by the VMAT planning method (16-19). Because of this, it is seem that the VMAT technique is more advantageous than IMRT.
CONCLUSION
According to our results, VMAT technique may be preffered instead of IMRT technique for breast cancer radiotherapy because it provides a lower MU than IMRT. We also recommend that each clinic make its own comparison for these results, which depend on the physical characteristics of the patient.
ORCIDs
NK: 0000-0001-9173-6280
SE: 0000-0001-9320-0391
CC BY License
This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/)
REFERENCES
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249. doi: 10.3322/caac.21660
- Ferlay J, Soerjomataram I, Ervik M, et al. GLOBACAN 2012 v1.0. Cancer incidence and mortality worldwide: IARC CancerBase No. 11. International Agency for Research on Cancer. Available from: http://globocan.iarc.fr
- Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med. 1997;337(14):949-955. doi: 10.1056/NEJM199710023371401
- Ragaz J, Jackson SM, Le N, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337(14):956-962. doi: 10.1056/NEJM199710023371402
- Effects of radiotherapy and surgery in early breast cancer — An overview of the randomized trials. N Engl J Med. 1995;333(22):1444-1456. doi: 10.1056/nejm199511303332202
- Rana S. Intensity modulated radiation therapy versus volumetric intensity modulated arc therapy. J Med Radiat Sci. 2013;60(3):81-83. doi: 10.1002/jmrs.19
- Johansen S, Cozzi L, Olsen DR. A planning comparison of dose patterns in organs at risk and predicted risk for radiation induced malignancy in the contralateral breast following radiation therapy of primary breast using conventional, IMRT and Volumetric modulated arc treatment techniques. Acta Oncologica. 2009;48(4):495-503. doi: 10.1080/02841860802657227
- Fong A, Bromley R, Beat M, Vien D, Dineley J, Morgan G. Dosimetric comparison of intensity modulated radiotherapy techniques and standard wedged tangents for whole breast radiotherapy. J Med Imaging Radiat Oncol. 2009;53(1):92-99. doi: 10.1111/j.1754-9485.2009.02043.x
- Peng G, Wang T, Yang KY, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol. 2012;104(3):286-293. doi: 10.1016/j.radonc.2012.08.013
- Kam MKM, Chau RMC, Suen J, et al. Intensity-modulated radiotherapy in nasopharyngeal carcinoma: dosimetric advantage over conventional plans and feasibility of dose escalation. Int J Radiat Oncol Biol Phys. 2003;56(1):145-157. doi: 10.1016/s0360-3016(03)00075-0
- Becker-Schiebe M, Stockhammer M, Hoffmann W, Wetzel F, Franz H. Does mean heart dose sufficiently reflect coronary artery exposure in left-sided breast cancer radiotherapy? : Influence of respiratory gating. Spiegelt die mittlere Herzdosis im Rahmen der Radiotherapie beim linksseitigen Mammakarzinom die Dosisbelastung der Koronararterien ausreichend wider? : Einfluss der Atemtriggerung. Strahlenther Onkol. 2016;192(9):624-631. doi: 10.1007/s00066-016-1011-y
- Lind PA, Wennberg B, Gagliardi G, Fornander T. Pulmonary complications following different radiotherapy techniques for breast cancer, and the association to irradiated lung volume and dose. Breast Cancer Res Treat. 2001;68(3):199-210. doi: 10.1023/a:1012292019599
- Grantzau T, Mellemkjær L, Overgaard J. Second primary cancers after adjuvant radiotherapy in early breast cancer patients: A national population based study under the Danish Breast Cancer Cooperative Group (DBCG). Radiother Oncol. 2013;106(1):42-49. doi: 10.1016/j.radonc.2013.01.002
- Travis LB. Therapy-associated solid tumors. Acta Oncol. 2002;41(4):323-333. doi: 10.1080/028418602760169361
- Thompson E, Mabuchi K, Ron E, et al. Cancer incidence in atomic bomb survivors. Part II: Solid tumors, 1958-1987. Radiat Res 1994;137(2 Suppl):S17-67
- Macklis R. In regards to Hall: Intensity-modulated radiation therapy, protons, and the risk of second cancers (Int J Radiat Oncol Biol Phys 2006;65:1–7). Int J Radiat Oncol Biol Phys. 2006;66(5):1593-1594. doi: 10.1016/j.ijrobp.2006.06.058
- Kry SF, Salehpour M, Followill DS, et al. The calculated risk of fatal secondary malignancies from intensity-modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2005;62(4):1195-1203. doi: 10.1016/j.ijrobp.2005.03.053
- Hoogeman MS, Nuyttens JJ, Levendag PC, Heijmen BJ. Time dependence of intrafraction patient motion assessed by repeat stereoscopic imaging. Int J Radiat Oncol Biol Phys. 2008;70(2):609-618. doi: 10.1016/j.ijrobp.2007.08.066
- Purdie TG, Bissonnette JP, Franks K, et al. Cone-beam computed tomography for on-line image guidance of lung stereotactic radiotherapy: localization, verification, and intrafraction tumor position. Int J Radiat Oncol Biol Phys. 2007;68(1):243-252. doi: 10.1016/j.ijrobp.2006.12.022
- Vala IS, Martins LR, Imaizumi N, et al. Low doses of ionizing radiation promote tumor growth and metastasis by enhancing angiogenesis. PloS One. 2010;5(6):e11222. doi: 10.1371/journal.pone.0011222
- Rüegg C, Monnier Y, Kuonen F, Imaizumi N. Radiation-induced modifications of the tumor microenvironment promote metastasis. Bull Cancer. 2011;98(6):47-57. doi: 10.1684/bdc.2011.1372
- Hall EJ, Wuu CS. Radiation-induced second cancers: the impact of 3D-CRT and IMRT. Int J Radiat Oncol Biol Phys. 2003;56(1):83-88. doi: 10.1016/s0360-3016(03)00073-7
- Kry SF, Salehpour M, Followill DS, et al. The calculated risk of fatal secondary malignancies from intensity-modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2005;62(4):1195-1203. doi:10.1016/j.ijrobp.2005.03.053
- Knapp P, Eva B, Reseigh G, et al. The role of volumetric modulated arc therapy (VMAT) in gynaecological radiation therapy: A dosimetric comparison of intensity modulated radiation therapy versus VMAT. J Med Radiat Sci. 2019;66(1):44-53. doi:10.1002/jmrs.311
- Adeneye S, Akpochafor M, Adedewe N, et al. A Dosimetric Comparison of Volumetric Modulated Arc Therapy and Intensity Modulated Radiotherapy in Patients Treated with Post-Mastectomy Radiotherapy. Eur J Breast Health. 2023;19(1):92-98. doi:10.4274/ejbh.galenos.2022.2022-9-2
- Mishra SS, Nanda S, Ahirwar MK, Simran, Rath SM. Advancing Precision in Post-mastectomy Chest Wall Radiotherapy: A Comparative Dosimetric Analysis of Volumetric-Modulated Arc Therapy (VMAT) and Intensity-Modulated Radiotherapy (IMRT) Based on Institutional Experience. Cureus. 2023;15(5):e38464. doi:10.7759/cureus.38464
- Canbolat HS. Dosimetric investigation of FIF, VMAT, IMRT, H-VMAT, and H-IMRT planning techniques in breast cancer radiotherapy. Turk J Oncol 2023;38(1):45–51. doi: 10.5505/tjo.2022.3740
- Peng G, Wang T, Yang KY, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol. 2012;104(3):286-293. doi:10.1016/j.radonc.2012.08.013
- Kam MK, Chau RM, Suen J, Choi PH, Teo PM. Intensity-modulated radiotherapy in nasopharyngeal carcinoma: dosimetric advantage over conventional plans and feasibility of dose escalation. Int J Radiat Oncol Biol Phys. 2003;56(1):145-157. doi:10.1016/s0360-3016(03)00075-0
- Kam MK, Leung SF, Zee B, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol. 2007;25(31):4873-4879. doi:10.1200/JCO.2007.11.5501
- Pow EH, Kwong DL, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys. 2006;66(4):981-991. doi:10.1016/j.ijrobp.2006.06.013
- Bedford JL. Treatment planning for volumetric modulated arc therapy. Med Phys. 2009;36(11):5128-5138. doi:10.1118/1.3240488
- Aznar MC, Petersen PM, Logadottir A, et al. Rotational radiotherapy for prostate cancer in clinical practice. Radiother Oncol. 2010;97(3):480-484. doi:10.1016/j.radonc.2010.09.014
- Sale C, Moloney P. Dose comparisons for conformal, IMRT and VMAT prostate plans. J Med Imaging Radiat Oncol. 2011;55(6):611-621. doi:10.1111/j.1754-9485.2011.02310.x
- Kinhikar RA, Pawar AB, Mahantshetty U, Murthy V, Dheshpande DD, Shrivastava SK. Rapid Arc, helical tomotherapy, sliding window intensity modulated radiotherapy and three dimensional conformal radiation for localized prostate cancer: a dosimetric comparison. J Cancer Res Ther. 2014;10(3):575-582. doi:10.4103/0973-1482.138200
- Peters S, Schiefer H, Plasswilm L. A treatment planning study comparing Elekta VMAT and fixed field IMRT using the varian treatment planning system eclipse. Radiat Oncol. 2014;9:153. doi:10.1186/1748-717X-9-153
- Yang R, Xu S, Jiang W, Xie C, Wang J. Integral dose in three-dimensional conformal radiotherapy, intensity-modulated radiotherapy and helical tomotherapy. Clin Oncol (R Coll Radiol). 2009;21(9):706-712. doi:10.1016/j.clon.2009.08.002
- Followill D, Geis P, Boyer A. Estimates of whole-body dose equivalent produced by beam intensity modulated conformal therapy [published correction appears in Int J Radiat Oncol Biol Phys 1997 Oct 1;39(3):783]. Int J Radiat Oncol Biol Phys. 1997;38(3):667-672. doi:10.1016/s0360-3016(97)00012-6
- Kry SF, Followill D, White RA, Stovall M, Kuban DA, Salehpour M. Uncertainty of calculated risk estimates for secondary malignancies after radiotherapy. Int J Radiat Oncol Biol Phys. 2007;68(4):1265-1271. doi:10.1016/j.ijrobp.2007.04.014
- Boice JD, Harvey EB, Blettner M, et al. Cancer in the Contralateral Breast after Radiotherapy for Breast Cancer. N Engl J Med. 1992;326(12):781-785. doi: 10.1056/nejm199203193261201
- Tubiana M. Can we reduce the incidence of second primary malignancies occurring after radiotherapy? A critical review. Radiother Oncol. 2009;91(1):4-3. doi:10.1016/j.radonc.2008.12.016
- Li Y, Wang J, Tan L, et al. Dosimetric comparison between IMRT and VMAT in irradiation for peripheral and central lung cancer. Oncol Lett. 2018;15(3):3735-3745. doi:10.3892/ol.2018.7732
- Kim DW, Chung K, Chung WK, et al. Risk of secondary cancers from scattered radiation during intensity-modulated radiotherapies for hepatocellular carcinoma. Radiat Oncol. 2014;9:109. doi:10.1186/1748-717X-9-109
